Tracheobronchial secretions are formed by mucous glands and goblet cells in man and many experimental animals; there is also an undetermined amount of transudation from serum. Estimates of the volume of the secretions in a normal human adult range from 10 to 100 cc/day. The secretions are composed of about 95 per cent water and 1 per cent each of carbohydrate, protein, lipid and inorganic material.
What is the volume of tracheobronchial secretions?
Tracheobronchial secretions are formed by mucous glands and goblet cells in man and many experimental animals; there is also an undetermined amount of transudation from serum. Estimates of the volume of the secretions in a normal human adult range from 10 to 100 cc/day.
Why is the consistency of tracheobronchial secretions important?
PHYSICAL PROPERTIES The consistency of the tracheobronchial secretions is of great importance in normal function and in abnormal states, but it has been very difficult to obtain measurements of the physical properties that may be relevant to conditions existing in vivo.
What is the meaning of tracheobronchial?
Definition of tracheobronchial. : of or relating to both trachea and bronchi. tracheobronchial lesions.
What is the catarrhal form of tracheobronchitis?
The catarrhal form of tracheobronchitis does not extend to the lungs, but is characterized by abundant mucus secretion and absence of obstruction. It can take an acute and chronic appearance. Most often it affects smokers and people working in conditions of high dust and gas contamination.

What are bronchial secretions?
Bronchial secretions are mainly produced by goblet cells and submucosal glands but also small amounts of surfactant from clara cells and some other fluids are part of the airway epithelium fluid.
What is secreted in the trachea?
Mucous and serous cells are found in the submucosal glands and epithelium of the trachea and large airways. These cells contribute to the secretion of airway mucus.
What secretes mucus in the trachea?
A moist tissue called mucosa lines each ring of tracheal cartilage. Mucosa have cells called goblet cells. Goblet cells produce a sticky substance called mucus. When you inhale, the mucus traps dust or other small debris to keep it from traveling to your lungs.
What can be the constituents of tracheobronchial secretion?
Tracheobronchial secretions are a complex mixture of secretory fluids derived from sources within the lung. Important constituents include the mucous glycoproteins, other secretory proteins, serum proteins, lipids, salts; water makes up 95% of mucus by weight.
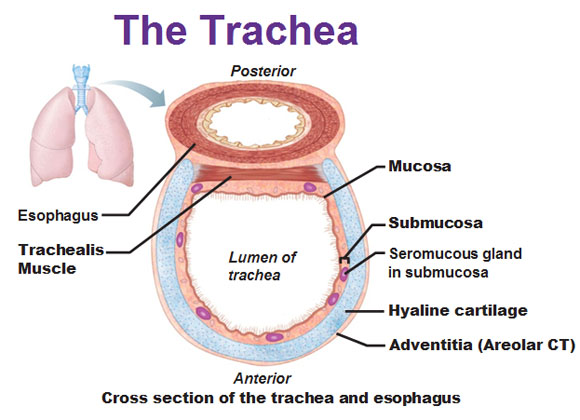
Does the trachea have mucous glands?
The trachea consists of four histological layers. The mucosa represents the innermost layer and it is lined with pseudostratified ciliated columnar epithelium. The second histological layer is the submucosa. It consists of connective tissue that contains mucus glands, smooth muscle, vessels, nerves and lymphatics.
Where does the mucus I cough up come from?
It's produced by mucous membranes that run from your nose to your lungs. Every time you breathe in, allergens, viruses, dust, and other debris stick to the mucus, which is then passed out of your system. But sometimes, your body can produce too much mucus, which requires frequent throat clearing.
What causes thick mucus secretions?
Your body usually makes thicker mucus when you have a cold (caused by viruses) or sinus infection (caused by bacteria). Most mucus problems are temporary. But producing too much mucus contributes to some serious conditions.
Where do you cough up mucus from?
The airways of the throat and lungs also produce mucus. And the body makes even more mucus when we're reacting to an allergy or have a cold or infection. If you're coughing up mucus, it's an indication that you have an irritation or possible infection in your respiratory tract.
Does the trachea carry food?
The trachea carries air directly into the lungs. The arrow shows the path of inspired air through the trachea. The esophagus is shown to the left of the trachea (it has been moved from its normal position dorsal to the trachea). It is the tube that carries food from the mouth to the stomach.
What is the function of the cilia in the trachea?
The bronchus in the lungs are lined with hair-like projections called cilia that move microbes and debris up and out of the airways. Scattered throughout the cilia are goblet cells that secrete mucus which helps protect the lining of the bronchus and trap microorganisms.
Which of the following is the function of trachea?
The primary function of the trachea is to transport air to and from the lungs. Without a trachea, a person would not be able to breathe. In addition to transporting air, the trachea helps defend against disease.
Can a person live without a trachea?
The lifespan of an infant born without a trachea is measured in minutes. Such a baby dies silently, having never drawn a breath. Only a few of these babies, and only because of extraordinary surgical interventions, have survived. In the United States, Thomas is the first.
Why do I cough when I have tracheobronchitis?
But because of the inflammatory process, the mucous membrane dries up, resulting in coughing, pain in the chest and increased production of mucus. It can be paroxysmal and become more frequent in the acute and chronic form of the disease. Very often, the main diagnosis and treatment plan depends on its type.
What are the effects of tracheal bronchitis?
In addition, there is a slight increase in temperature, which lasts a long period of time and sputum production. Patients feel general weakness, aches in the whole body and painful sensations behind the sternum. This all happens against the background of a decrease in appetite and attacks of dry cough.
What is the condition that causes a small sputum discharge?
Most often, chronic tracheobronchitis affects people who work in conditions of high dust (miners) or who have bad habits (smoking, alcoholism). The chronic form is characterized by a paroxysmal dry cough with a small sputum discharge. The disease causes accompanying pathologies (sinusitis, rhinitis, sinusitis) and can last more than three months.
Why does the upper respiratory tract have a long recovery period?
In this case, therapy is a long process and a long recovery period, since the body has been exposed to microbial activity, and gas exchange has been disturbed in the lungs. The patient suffers from fever and a strong cough that occurs both during the day and at night.
What are the symptoms of a barrel thorax?
As for the symptoms of the obstructive form, it is a cough and shortness of breath, heavy, wheezing, fever. Diagnosis begins with an examination. Due to prolonged inflammatory process, the thorax acquires a barrel shape, possibly a swelling of the supraclavicular spaces and swelling of the cervical veins.
What is a tracheobronchial?
Medical Definition of tracheobronchial. : of, relating to, affecting, or produced in the trachea and bronchi tracheobronchial secretion tracheobronchial lesions.
How many dogs are trained to detect saliva?
Recent Examples on the Web The team used eight dogs trained for a week to detect saliva or tracheobronchial secretions, from SARS-CoV-2 positive patients. — Nancy Clanton, ajc, 30 July 2020
Where is the trachea located?
The trachea originates at the inferior edge of the larynx and connects to the left and main stem bronchus. The primary function of the trachea is to allow passage of inspired and expired air into and out of the lung. The trachea is a midline structure and lies just anterior the esophagus.
What is the tree of the trachea?
The tracheobronchial tree is composed of the trachea, the bronchi, and the bronchioles that transport air from the environment to the lungs for gas exchange.
Why is the trachea cartilage incomplete?
The main reason why the C-shaped cartilage rings are incomplete is that they allow the trachea to narrow. This action is helpful, especially when eating food, which requires the expansion of the esophagus.
What is the trachea divided into?
After it originates from the larynx, the trachea divides into the left and right mainstem bronchi. This junction point is called the carina. The tracheal diameter is about 24 to 26 mm in adult males and 22 to 24 mm in females. It is much broader in the proximal area than the distal segment. The trachea is 16 to 20 C-shaped cartilage rings stacked one on top of another. A narrow thin membrane connects each of the tracheal rings. The posterior aspect of the trachea is adjacent to the anterior esophagus.
How many layers does the trachea have?
The trachea has four layers. The inner mucosal layer has a lining of ciliated pseudostratified columnar epithelium with goblet cells. These cells are responsible for secreting mucus which coats the inner lining of the trachea. The mucus traps dust particles and other debris before they reach the lung. The cilia function to propel the dust away from the lung.
When does the respiratory tract develop?
Lower respiratory tract development begins on day 22 and divides into five stages: embryonic, pseudoglandular, canalicular, saccular, and alveolar. Although the development of the respiratory tract begins early in fetal development, complete maturation does not occur until approximately the eighth year of life.
How to remove secretions from a patient?
The most convenient way to remove most secretions is coughing. So it is necessary to assist the patient during this activity. Deep breathing, on the other hand, promotes oxygenation before controlled coughing.
What is labored breathing?
Labored breathing may be a sign of respiratory infection that needs an appropriate treatment of antibiotics. Use pulse oximetry to monitor oxygen saturation; assess arterial blood gases (ABGs) Pulse oximetry is used to detect changes in oxygenation. Oxygen saturation should be maintained at 90% or greater.
What are the common goals and expected outcomes for Ineffective Airway Clearance?
The following are the common goals and expected outcomes for Ineffective Airway Clearance. Patient will maintain clear, open airways as evidence by normal breath sounds, normal rate and depth of respirations, and ability to effectively cough up secretions after treatments and deep breaths.