There are a host of factors that can cause the acquired form of keratoderma, some of which include: Infections Medications and drugs Various skin disorders
- Infections
- Medications and drugs
- Various skin disorders
What is acquired keratoderma?
Acquired keratoderma is a palmoplantar keratoderma that is NOT inherited as a primary genetic condition. It may occur as part of a generalised skin condition (some of which may be inherited) or as a result of another illness.
What causes palmoplantar keratoderma (PPK)?
Palmoplantar keratoderma (PPK) can be either acquired during the lifetime (more commonly) or inherited. Acquired PPK may arise due to changes in a person's health or environment. Inherited forms of PPK are caused by genetic mutations that result in abnormalities of keratin (a skin protein).
What is the most common cause of keratoderma climactericum?
Keratoderma climactericum occurs more commonly in women of menopausal age with no personal or family history of skin diseases. Hormonal imbalance may play a role as well as obesity, hypertension, cold dry climates and wearing backless shoes, e.g. sandals.
What are the different types of keratoderma?
Diffuse: Also known as Vorner’s disease, this condition tends to result in a uniform pattern of keratoderma across the skin of the soles and palms. Punctate: With this form of palmoplantar keratoderma, numerous small nodules appear all over the soles. This condition tends to cause more pain in weight-bearing parts of the foot.
How do you get keratoderma?
Keratoderma may be inherited (hereditary) or, more commonly, acquired. The hereditary keratodermas are caused by a gene abnormality that results in abnormal skin protein (keratin). They may be inherited either by an autosomal dominant or autosomal recessive pattern.
How do you get rid of keratoderma?
Palmoplantar keratoderma, an inherited condition, cannot be cured, but its symptoms can be controlled. Individuals who have keratoderma also undergo stress due to the appearance of their skin, which affects their mental health.
How do you get palmoplantar keratoderma?
1) Mal de Meleda It was initially observed in inhabitants of the Adriatic island of Meleda (Miljet). It is transmitted through an autosomal recessive inheritance. Clinical features of the disorder usually appear in early infancy. Palmoplantar keratoderma is often the only manifestation.
Is keratoderma autoimmune?
1 Palmoplantar keratodermas (PPKs) are characterized by hyperkeratosis of the skin on the palms and soles. 2 Multiple cases have been reported associating PPK with autoimmune thyroiditis.
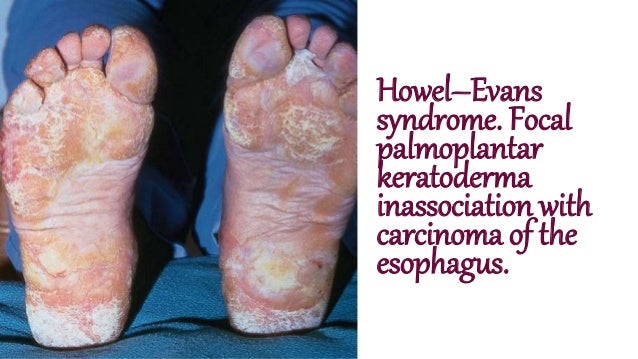
What is the cause of Tylosis?
Genetic Disease. Tylosis with esophageal cancer is a genetic disease, which means that it is caused by one or more genes not working correctly.
Is keratoderma itchy?
Besides involvement of the palms and soles, manifesting by hyperkeratotic layers, painful fissures and itching, the patients with climacteric keratoderma develop metabolic endocrine, neurovegetative, and psychoemotional disorders.
Is palmoplantar keratoderma rare?
Punctate palmoplantar keratoderma type I is a rare condition that affects the skin. It is a sub-type of punctate palmoplantar keratoderma. Signs and symptoms typically begin in early adolescence or later and include hard, round bumps of thickened skin on the palms of the hands and soles of the feet.
Is palmoplantar keratoderma common?
Isolated palmoplantar keratodermas are the most common and primarily involve the palms and soles. Due to the sheer breadth of this topic, I will be focusing on the isolated varieties. We can further distill all palmoplantar keratodermas into diffuse, focal, striate (palms) and punctate forms.
What causes thick skin on hands and feet?
Hyperkeratosis is a thickening of the outer layer of the skin. This outer layer contains a tough, protective protein called keratin. This skin thickening is often part of the skin's normal protection against rubbing, pressure and other forms of local irritation. It causes calluses and corns on hands and feet.
Is Palmoplantar Keratoderma painful?
Pain is a prominent symptom in hereditary palmoplantar keratodermas (PPKs). Pain in patients with PPK can be difficult to treat. Pain mechanisms in PPKs are poorly understood.
Is hyperkeratosis hereditary?
Epidermolytic hyperkeratosis is usually inherited in an autosomal dominant pattern. This means that one copy of a mutated gene is able to cause the disorder and can be inherited from either parent. If one parent is affected, each child has a 50% chance of inheriting the disease.
What is Aquagenic keratoderma?
Aquagenic keratoderma (AK) is a rare acquired skin condition characterized by recurrent and transient white papules and plaques associated with a burning sensation, pain, pruritus and/or hyperhidrosis on the palms and more rarely, soles triggered by sweat or contact with water.
What is Aquagenic keratoderma?
Aquagenic keratoderma (AK) is a rare acquired skin condition characterized by recurrent and transient white papules and plaques associated with a burning sensation, pain, pruritus and/or hyperhidrosis on the palms and more rarely, soles triggered by sweat or contact with water.
How do you treat keratosis Punctata?
Treatment options include topical keratolytics, emollients and occasionally systemic retinoids for severe cases. Systemic retinoids, such as etretinate, carry the risk of associated side effects such as hepatotoxicity.
What is Keratoderma Blennorrhagica?
Keratoderma blennorrhagica, a thickening and keratinization of the skin that generally involves the feet, hands, and nails that resemble psoriasis clinically and on histopathology.
What is punctate keratoderma?
Punctate palmoplantar keratoderma type I is a rare condition that affects the skin. It is a sub-type of punctate palmoplantar keratoderma. Signs and symptoms typically begin in early adolescence or later and include hard, round bumps of thickened skin on the palms of the hands and soles of the feet.
Can Palmoplantar Keratoderma Be Cured?
Palmoplantar keratoderma, an inherited condition, cannot be cured, but its symptoms can be controlled. Individuals who have keratoderma also underg...
Can Palmoplantar Keratoderma Spread From One Person to Another?
An autosomal recessive inheritance can transmit the palmoplantar keratoderma. But, it is not contagious or infectious.
What Do You Mean by Acquired Keratoderma?
Acquired keratoderma is the keratoderma which is not inherited. It is usually acquired by a generalized skin condition or by another illness.
What Do You Mean by Keratosis Punctata?
Keratosis punctata is a rare disorder that commonly occurs in the skin of black people. In this, the lesion will have 1 to 5 mm of depression, whic...
How Do You Treat Palmoplantar Keratoderma?
Treatment aims to reduce the thickness of the skin and softening the skin. Treatment options include regular use of saltwater soaks, emollients, to...
How to Cure Palmoplantar Psoriasis?
Palmoplantar psoriasis is a long-term condition, and it cannot be cured, but the symptoms can be controlled. They can be treated with: - Topical st...
What Diet Should You Follow in Palmoplantar Keratoderma?
The diet to be followed in palmoplantar keratosis is to avoid all spicy and salty foods, which can ease psoriasis symptoms.
What Is the Differential Diagnosis for Palmoplantar Keratoderma?
The differential diagnosis for palmoplantar keratoderma are: - Tinea pedis. - Psoriasis. - Contact dermatitis. - Reactive arthritis. - Atopic derma...
What Surgery Can Be Done for Palmoplantar Keratoderma?
The surgical treatment for palmoplantar keratoderma includes full-thickness excision of the hyperkeratotic plaques, followed by skin grafting.
Is Palmoplantar Keratoderma associated with Lung Cancer?
Palmoplantar keratoderma is a congenital or acquired disorder characterized by abnormal thickening of the skin of the sole and palm. The thickening...
What is focal keratoderma?
Focal keratodermas mainly affect pressure areas. Punctate -type keratoderma results in tiny bumps on the palms and soles. Most often the abnormal skin involves only the palms and soles (non-transgradient palmoplantar keratoderma) but sometimes it extends on to the top of the hands and feet as well (transgradient).
What is the difference between palmoplantar keratoderma and focal keratoderma?
Diffuse keratodermas affect most of the palms and soles. Focal keratodermas mainly affect pressure areas.
How many chances are there of having autosomal recessive keratodermas?
If one parent is affected there is a 50% chance that each child will be affected. Autosomal recessive keratodermas occur less commonly within an affected family. This is because both parents need to pass on an abnormal gene to the child for it to be affected.
Is keratoderma hereditary?
Keratoderma may be inherited ( hereditary) or, more commonly, acquired. Hereditary keratoderma: the condition runs in families and is passed down or from one or both parent (s) to their children. The hereditary keratodermas are caused by a gene abnormality that results in abnormal skin protein ( keratin ).
Is keratoderma focal or diffuse?
Marginal keratoderma (acrokeratoelastoidosis, autosomal dominant) Acquired palmoplantar keratodermas may be focal or diffuse. They may arise in association with a variety of different skin and internal conditions. An inflammatory skin condition (eg, eczema or psoriasis) Infections. Medications and toxins.
What is the condition that causes a uniform pattern of keratoderma on the skin of the soles and
Diffuse: Also known as Vorner’s disease, this condition tends to result in a uniform pattern of keratoderma across the skin of the soles and palms. Punctate: With this form of palmoplantar keratoderma, numerous small nodules appear all over the soles.
Where does palmoplantar keratoderma affect the skin?
All varieties of palmoplantar keratoderma can affect both the hands and the feet, but focal palmoplantar keratoderma tends mostly to affect the skin on the bottom of the foot.
What is the difference between palmoplantar keratoderma and diffuse keratoderma?
There are three general classifications of palmoplantar keratoderma: Focal: With this condition, the keratoderma appears at pressure points, i.e., areas of the feet that bear significant weight or that are subject to friction when we walk. Diffuse: Also known as Vorner’s disease, this condition tends to result in a uniform pattern ...
What is palmoplantar keratoderma?
A Complete Guide To Palmoplantar Keratoderma. The term palmoplantar keratoderma describes a diverse group of skin conditions affecting the hands and feet—specifically the palms and the soles (also known as the plantar region of the foot, hence the name “palmo- plantar keratoderma”). Keratoderma means “thickened skin.”.
Is keratoderma congenital?
Affected individuals suffer calluses and blisters so painful that they experience difficulty walking. Most varieties of this condition are congenital—and usually inherited—although there are acquired forms as well.
Is palmoplantar keratoderma a genetic condition?
While palmoplantar keratoderma is in most cases a genetic condition, there are situations in which it can be acquired, usually as a symptom of some inflammatory skin condition, such as psoriasis, eczema, ichthyosis, scabies, or dermatitis.
What causes PPK to be inherited?
Inherited forms of PPK are caused by genetic mutations that result in abnormalities of keratin (a skin protein ). These forms of PPK may be present in more than one family member. Mutations in several genes can cause an inherited form of PPK.
What causes PPKs to be autosomal dominant?
Inherited PPKs are caused by genetic mutations that result in abnormalities of keratin, a skin protein. Depending on the genetic cause, inheritance can be autosomal dominant or autosomal recessive. [1] [2] Treatment is aimed at softening the thickened skin to make it less noticeable and relieve discomfort. [2]
Who gets Acquired Keratoderma? (Age and Sex Distribution)
Acquired Keratoderma may be observed in a wider age range of individuals
What are the Risk Factors for Acquired Keratoderma? (Predisposing Factors)
Acquired Keratoderma occur secondary to infections, medication use, chronic inflammatory conditions, circulatory disorders, and many other factors
What are the Causes of Acquired Keratoderma? (Etiology)
Acquired Keratoderma is caused by several diseases, conditions, or medications that are listed below:
What are the Signs and Symptoms of Acquired Keratoderma?
The signs and symptoms associated with Acquired Keratoderma may include:
What are the possible Complications of Acquired Keratoderma?
Complications associated with Acquired Keratoderma include complications associated with the cause of the condition.
How is Acquired Keratoderma Treated?
The treatment of Acquired Keratoderma is based upon the underlying cause of the condition. However, the skin thickening may be addressed through skin softening treatment measures such as:
How can Acquired Keratoderma be Prevented?
The prevention of Acquired Keratoderma depends upon the underlying cause of the skin condition. It may not be preventable in a majority of individuals
What is keratoderma climactericum?
Keratoderma climactericum refers to the form that occurs during the menopausal period. What causes keratoderma climactericum? Keratoderma climactericum occurs more commonly in women of menopausal age with no personal or family history of skin diseases.
What is the term for the development of harmless skin thickening on the soles of the feet?
Keratoderma climactericum. Also known as Haxthausen disease. What is keratoderma climactericum? There are many forms of keratoderma which is the term given to the development of harmless skin thickening on the soles, particularly the heels. Keratoderma climactericum refers to the form that occurs during the menopausal period.
What are the genes that cause keratoderma?
Mutations in the JUP, DSP, DSC2, and KANK2 genes cause keratoderma with woolly hair types I through IV, respectively. The JUP, DSP, and DSC2 genes provide instructions for making components of specialized cell structures called desmosomes. Desmosomes are located in the membrane surrounding certain cells, including skin and heart muscle cells. Desmosomes help attach cells to one another, which provides strength and stability to tissues. They also play a role in signaling between cells.
What are the complications of keratoderma with woolly hair?
Complications of cardiomyopathy can include an abnormal heartbeat (arrhythmia), heart failure, and sudden death. Keratoderma with woolly hair comprises several related conditions with overlapping signs and symptoms. Researchers have recently proposed classifying keratoderma with woolly hair into four types, based on the underlying genetic cause.
What causes skin on the palms of the hands and the soles of the feet to become thick, scal
Starting early in life, affected individuals also develop palmoplantar keratoderma, a condition that causes skin on the palms of the hands and the soles of the feet to become thick, scaly, and calloused. Cardiomyopathy, which is a disease of the heart muscle, is a life-threatening health problem that can develop in people with keratoderma ...
Is keratoderma with woolly hair rare?
Keratoderma with woolly hair is rare; its prevalence worldwide is unknown. Type I (Naxos disease) was first described in families from the Greek island of Naxos. Since then, affected families have been found in other Greek islands, Turkey, and the Middle East.
Can keratoderma cause woolly hair?
Cardiomyopathy, which is a disease of the heart muscle, is a life-threatening health problem that can develop in people with keratoderma with woolly hair. Unlike the other features of this condition, signs and symptoms of cardiomyopathy may not appear until adolescence or later.
Does keratoderma have autosomal recessive inheritance?
Most cases of keratoderma with woolly hair have an autosomal recessive pattern of inheritance, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they usually do not show signs and symptoms of the condition.
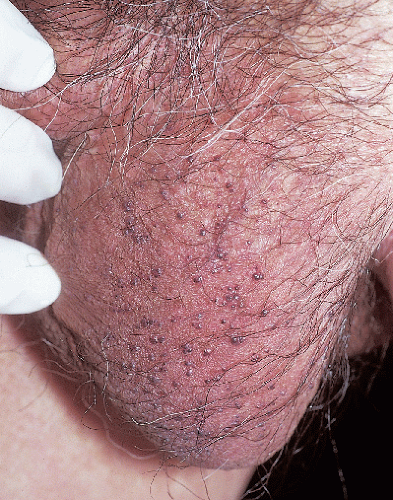
When are you more likely to develop keratosis?
Risk factors. You're generally more likely to develop seborrheic keratoses if you're over age 50. You're also more likely to have them if you have a family history of the condition. By Mayo Clinic Staff.
Where does seborrheic keratosis appear?
It typically appears on the face, chest, shoulders or back. You may develop a single growth, though multiple growths are more common. A seborrheic keratosis: Ranges in color from light tan to brown or black. Is round or oval shaped. Has a characteristic "pasted on" look. Is flat or slightly raised with a scaly surface.
How big can a seborrheic keratosis grow?
Some can grow large, up to 1 inch (2.5 centimeters) across . Seborrheic keratoses are usually round or oval and range in color from light tan to black. They can develop as a single growth or in clusters. A seborrheic keratosis (seb-o-REE-ik ker-uh-TOE-sis) is a common noncancerous skin growth.
What is the name of the waxy dark brown keratose on the back?
Seborrheic keratoses on the back. Seborrheic keratoses on the back. Seborrheic kera toses are very common on the back. They appear as waxy light tan, brown or black growths that look as if they were dripped onto the skin by a candle. Some can grow large, up to 1 inch (2.5 centimeters) across.
Is a keratosis on the head contagious?
They usually appear on the head, neck, chest or back. Seborrheic keratoses are harmless and not contagious. They don't need treatment, but you may decide to have them removed if they become irritated by clothing or you don't like how they look.
Is seborrheic keratosis a single growth?
They can develop as a single growth or in clusters. A seborrheic keratosis (seb-o-REE-ik ker-uh-TOE-sis) is a common noncancerous skin growth. People tend to get more of them as they get older. Seborrheic keratoses are usually brown, black or light tan. The growths look waxy, scaly and slightly raised. They usually appear on the head, neck, chest ...