What are lumbosacral transitional vertebrae?
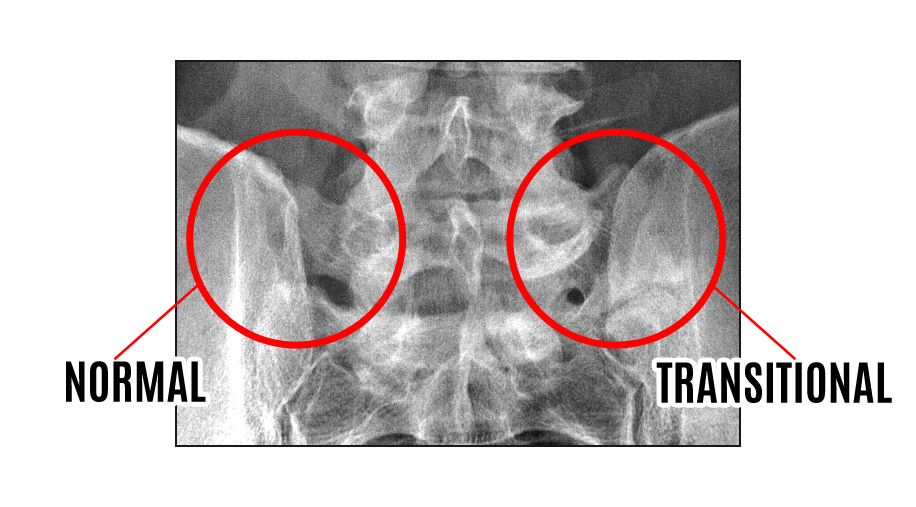
Lumbosacral transitional vertebrae (LSTV) are congenital spinal anomalies, in which an elongated transverse process of the last lumbar vertebra fuses with varying degree to the “first” sacral segment.
What is a transitional vertebra?
A transitional vertebra is a somewhat common lumbosacral spinal abnormality in which one spinal bone does not form correctly and definitively as a lumbar segment or a sacral segment. Instead, the vertebral body takes on characteristics of both typical lumbar and sacral spinal bones; but does not truly represent either variety in totality.
What is sacralization of L5 vertebrae?
The fifth lumbar vertebra, known as L5, may fuse fully or partially on either side of the sacrum, or on both sides. Sacralization is a congenital anomaly that occurs in the embryo.
What year was the partial lumbosacral transitional vertebrae resection?
(2001) Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine. 26(2):226–9. (2012) Prediction of transitional lumbosacral anatomy on magnetic resonance imaging of the lumbar spine.
How do you treat transitional vertebrae?
Options include surgical removal of the transitional segment, decompression of stenosed foramina, and spinal fusion. Recent evidence suggests that radiofrequency ablation (RFA) around the transitional segment may also provide relief.
How common is lumbosacral transitional vertebrae?
Overview of Literature. LSTV is the most common congenital anomaly of the lumbosacral spine. The prevalence has been debated to vary between 7% and 30%, and its relationship to back pain, disc degeneration and herniation has also not been established.
Is transitional vertebrae hereditary?
Different types of LTV exist and radiographic screening is used to determine the form of LTV in dogs. The disorder can be seen right after birth and it is hereditary.
What does a transitional vertebra mean?
A transitional vertebra is one that has indeterminate characteristics and features of vertebrae from adjacent vertebral segments. They occur at the junction between spinal morphological segments: atlanto-occipital junction.
How do you fix Bertolotti syndrome?
Spine-specialized physical therapy helps with mobilization, core strengthening, and stretching. Other options include steroid injections, radiofrequency ablation, and regenerative treatments such as prolotherapy and platelet rich plasma (PRP). For some patients surgical intervention may be necessary.
Can lumbarization cause back pain?
Typically, patients with lumbarization of the spine can experience pain during movement. This can cause a great deal of difficulty when performing activities of daily living.
What is a transitional vertebra at L5?
“Transitional vertebra” is a fairly common spinal deformity, in which the lowest vertebrae of the spine, the fifth lumbar vertebra, is partially fused to the top of sacrum. This odd hybrid bone is not a proper lumbar vertebra, and certainly not a sacral segment either — thus, it is a “transitional” vertebra.
Does having an extra vertebrae cause problems?
Having a sixth lumbar vertebrae in your spine is uncommon, but far from extraordinary. About 10% of the population has an extra bone in this region. While additional vertebrae don't typically affect your health, they can complicate treatment for spinal cord injuries.
How can you tell between L5 and S1?
The L5 and S1 vertebrae have different features:L5 consists of a vertebral body in front and an arch in the back that has 3 bony protrusions: a prominent spinous process in the middle and two transverse processes on the sides. ... S1, also called the sacral base, is the upper and wider end of the triangular-shaped sacrum.More items...
Are you born with Bertolotti Syndrome?
Bertolotti's syndrome is a commonly missed cause of back pain which occurs due to lumbosacral transitional vertebrae (LSTV). It is a congenital condition but is not usually symptomatic until one's later twenties or early thirties.
Does Bertolotti syndrome get worse?
CONCLUSIONS. Patients with Bertolotti syndrome undergo significantly longer workup and more ESIs and have worse physical and mental health scores than age- and sex-matched patients with lumbosacral radiculopathy.
How is Bertolotti Syndrome diagnosed?
Bertolotti syndrome can be diagnosed based upon a good medical history, a thorough physical exam and X-rays. The physical exam will include recreating the movements that trigger pain or discomfort. Then, an X-ray of the lower back and pelvis can reveal any bony anatomy abnormalities.
How common is sacralization of L5?
Incidence. Estimates of the incidence of sacralization in the general population vary widely, from 4 to 36 percent. The wide range of estimates is attributed to differences of diagnostic methods and definition. Among people under 30, an estimated 18.5 percent have sacralization.
Is Bertolotti Syndrome a disability?
Along with significant pain, patients with Bertolotti's Syndrome self-report an average of over 36% on the Oswestry disability scale, correlating to a moderate disability that affects many aspects of daily life.
How do you treat sacralization of L5?
Treatment for SacralizationLifestyle modifications to avoid or change activities that increase pain.Over the counter (OTC) pain medication, as directed.Physical therapy.Periodic treatment, such as steroid injections to reduce symptoms.More items...•
Is Sacralization congenital?
Sacralization is a congenital vertebral anomaly of the lumbosacral spine (fusion between L5 and the first sacral segment) [1]. This alteration may contribute to incorrect identification of a vertebral segment.
What is a lumbosacral transitional vertebrae?
Lumbosacral transitional vertebrae (LSTV) are increasingly recognized as a common anatomical variant associated with altered patterns of degenerative spine changes. This review will focus on the clinical significance of LSTV, disruptions in normal spine biomechanics, imaging techniques, diagnosis, and treatment.
What is the association between LSTV and morphological alterations of neural arch elements and auricular surfaces?
The association between LSTV with morphological alterations of neural arch elements and auricular surfaces is well established. Considering the biomechanical importance of these morphological alterations in maintaining stability of the lumbar spine, Mahato suggests re-defining and modifying the current classification of LSTV. Including facet and auricular surface status would allow clinicians to clearly delineate the entire range of information required to visualize and clinically interpret any subtype of LSTV affliction (Table 1).2
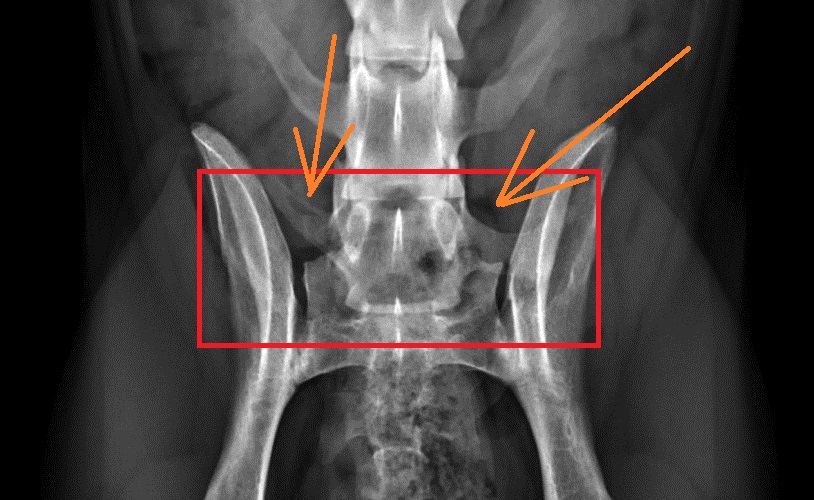
What is LSTV in spine?
LSTV are associated with alterations in biomechanics and anatomy of spinal and paraspinal structures, which have important implications on surgical approaches and techniques. LSTV are often inaccurately detected and classified on standard AP radiographs and MRI. The use of whole-spine images as well as geometric relationships between the sacrum and lumbar vertebra increase accuracy. Uncertainty regarding the cause, clinical significance, and treatment of LSTV persists. Some authors suggest an association between LSTV types II and IV and low back pain. Pseudoarticulation between the transverse process and the sacrum creates a “false joint” susceptible to arthritic changes and osteophyte formation potentially leading to nerve root entrapment.
What is the prevalence of LSTV?
Estimates of the prevalence of LSTV in the general population vary widely throughout the literature due to differences in definition and diagnostic modalities, ranging from 4.0% -35.9% with a mean of 12.3%.3, 5, 7, 8In a study of 211 participants, Apazidis et al. determined Type IA most common with a prevalence of 14.7%;7however, Type I is generally considered to have no clinical significance and does not require further attention in clinical practice.6In an asymptomatic population, Nardo et al. determined that Type I and Type II were each responsible for more than 40% of total occurrences of LSTV, while Type III and Type IV accounted for 11.5% and 5.25% of occurrences, respectively.9In unilaterally occurring malformations, the incidence is significantly higher on the left side, a finding which remains unexplained.10
What is the weak iliolumbar ligament?
The weak iliolumbar ligaments result in vertebral segment instability and could subsequently lead to early disc degeneration. The formation of an articulation or boney union between vertebra and sacrum through the transverse process may represent an adaptive mechanism to compensate for a weak iliolumbar ligament and to preserve stability.20
Which facet is present on the side of the L5 enlargement?
With presence of ipsi/contra lateral rudimentary facet to the side of the L5 enlargement
Which structure is responsible for dissipating weight from the upper body toward the sacroiliac joint?
The sacrum, lying at the base of the vertebral column, optimizes the dissipation of the weight of the upper body toward the sacroiliac (SI) joint by working as a fused mass of boney elements.11The sacrum's ability to dissipate load depends on its size and its surface area with the SI joint.
What is a transitional lumbar vertebrae?
A Transitional Lumbosacral Vertebrae is condition that occurs when the last vertebrae in the spine is improperly formed. It creates a situation where the number of vertebrae in the lower back is either increased by one or decreased by one. The normal number of vertebrae in the lower back, or lumbar spine is 5. When a Transitional Lumbosacral Vertebrae is present, you have either 4 lumbar vertebrae, making the spine shorter than usual or 6 lumbar vertebrae making the spine longer than usual. In addition to changes in the number of vertebrae and the overall length of the spine, the Transitional Lumbosacral Vertebrae is typically malformed. It takes on the structural characteristics of both a vertebrae and the sacrum..... while forming in the womb, it could not make up its mind which one to become so it became a little of both.
Is the disc under a transitional lumbosacral vertebrae unformed?
The disc under a Transitional Lumbosacral Vertebrae is typically unformed and very thin
How many vertebrae are there in the human spine?
These vertebral anomalies a …. Human lumbar spine usually consists of five vertebrae; however, some individuals have vertebral anomalies with four or six lumbar vertebrae because of sacralized fifth lumbar vertebra (L5 sacralization) or lumbarized first sacral vertebra (S1 lumbarization), respectively. These vertebral anomalies a ….
Is LSTV an anomaly?
Although LSTV is an asymptomatic anomaly, it is known to cause misconception in spinal counts and in spinal level at lumbar spinal surgery. The purpose of this study is to evaluate how LSTV affects the diagnosis and surgeries in lumbar spine disorders.
What is the lumbar transitional vertebra?
Lumbosacral transitional vertebra is an anatomical variation of the fifth lumbar vertebra in which an enlarged transverse process can form a joint or fusion with the sacrum or ilium. The association of that variant with low back pain and the change in the biomechanical properties of the lumbar spine is called Bertolotti’s syndrome.
Which transitional vertebra causes Bertolotti's syndrome?
Lumbosacral transitional vertebra causing Bertolotti’s syndrome: a case report and review of the literature
Why is the L5-S1 disc protected?
Luoma et al hypothesized that because of the restriction of rotational and bending movements by the pseudarthroses the L5-S1 disc is protected from traumatic events [5]. According to Castellvi et al the transitional vertebrae cause abnormal torque movements above these anomalous vertebrae, a fact that could result in disc degeneration [2]. Aihara et al in an anatomical study of 70 cadavers claimed that the iliolumbar ligament at the level immediately above the transitional vertebra is much thinner and weaker than in cadavers without a lumbosacral transitional vertebra. Especially the posterior bands of the ligament at this level have the appearance of fascia rather than of a ligament. Due to that condition disc degeneration may occur at higher vertebral levels more frequently than level L5-S1. The same authors found the iliolumbar ligaments at the lumbosacral transitional vertebra consisting of dense fibrous connective tissue, thus protecting the L5-S1 disc [11].
What is Bertolotti's syndrome?
Introduction. “Bertolotti’s syndrome” is characterised by the presence of a variation of the fifth lumbar vertebra having a large transverse process, either articulated or fused with the sacral basis or iliac crest, and producing a chronic, persistent low back pain [1,2]. Bertolotti stated as early as in 1917 that these abnormal vertebrae may ...
Does the transitional vertebra cause nerve root pain?
Otani et al supported that the transitional vertebra does not influence the incidence of nerve root symptoms. However, they claimed that this vertebra in patients with disc herniation or lumbar canal stenosis without spondylolisthesis may be a risk factor for the development of nerve root symptoms [10]. Quinlan et al found the total incidence of Bertolotti’s syndrome being 4.6%, while the frequency was 11.4% in under 30-year age group. These authors claimed that the transitional vertebra should be kept in mind when low back pain is appeared in young individuals [6]. Vergauwen et al demonstrated that the abnormal vertebra does not constitute a risk factor for spine degenerative changes, but when degeneration occurs it is focused on the suprajacent level of the transitional vertebra [4]. In our case we consider that the localized pain was caused by the degenerative changes of the anomalous articulation between the transverse process of the transitional vertebra and the ala sacrum.
Is Bertolotti's syndrome a differential diagnosis?
The list of differential diagnosis should always include Bertolotti’s syndrome, when investigating back pain in young patients. The treatment, whether conservative or operative, is still debated. In our case we performed injection with local anesthetic and steroid within the abnormal articulation and after a follow-up of 18 months patient reported an improvement of his symptoms, however not complete resolution.
Can a transitional vertebra cause sciatica?
Whether such an anatomical variation produces or not low back pain and/or sciatica is a subject of great debate. Some authors believe that the lumbosacral transitional vertebra could cause symptoms of back pain and/or sciatica [1,4,6,7], while others claim that this abnormal vertebra does not affect their incidence [5,8,9].
What is transitional vertebra?
A transitional vertebra is a somewhat common lumbosacral spinal abnormality in which one spinal bone does not form correctly and definitively as a lumbar segment or a sacral segment. Instead, the vertebral body takes on characteristics of both typical lumbar and sacral spinal bones; but does not truly represent ...
What is the transitional spinal bone?
There are a variety of forms of transitional spinal bones. Most often, the occurrence of an extra vertebra is demonstrated and is often named L6 . Sometimes the usual L5 is replaced by a transitional segment and other times, the usual S1 is replaced by a transitional segment. Occasionally, transitional spinal bones can also occur at the cervicothoracic juncture, as well.
Does transitional spinal bone cause sciatica?
Many studies have been done on transitional spinal bones and most have found no correlation with lower back pain or sciatica. Some studies have found links, but most of these were investigating a specific treatment for the condition, so their objectivity may be suspect.
Can a transitional spinal segment cause pain?
If you have a transitional spinal segment in your lower back or neck, it is certainly possible that it is causing you some pain. This is true for any vertebra, even if it is formed correctly.
Is transitional segment pain a symptom?
The vast majority are not problematic and statistically do not cause pain. However, in uncommon instances, there might be a pathological component to a transitional segment which may make it symptomatic.
Can transitional spinal bones be seen at the cervicothoracic juncture?
Occasionally, transitional spinal bones can also occur at the cervicothoracic juncture, as well. Transitional spinal segments can be diagnosed using advanced imaging technologies and are not usually any cause for concern. The vast majority are not problematic and statistically do not cause pain.
What is a lumbosacral transitional vertebrae?
Background Lumbosacral transitional vertebrae (LSTV) are increasingly recognized as a common anatomical variant associated with altered patterns of degenerative spine changes. This review will focus on the clinical significance of LSTV, disruptions in normal spine biomechanics, imaging techniques, diagnosis, and treatment.
Why does LSTV cause pain?
Bertolotti stated as early as 1917 that an LSTV may produce low back pain due to arthritic changes occurring at the site of pseudoarthrosis. 36 Pain in the presence of an LSTV may also arise from disc herniation or degeneration, facet joint arthrosis, or spinal canal or foraminal stenosis. 5 In 1989, Elster et al.'s radiographic study of 2000 patients suggested that the overall incidence of structural pathology, including significant disc protrusion, nerve root canal stenosis, spondylolysis, and sclerosis at “false joints” is not appreciably higher in LSTV patients than in patients without such vertebrae. 37
What is LSTV associated with?
The association between LSTV with morphological alterations of neural arch elements and auricular surfaces is well established. Considering the biomechanical importance of these morphological alterations in maintaining stability of the lumbar spine, Mahato suggests re-defining and modifying the current classification of LSTV. Including facet and auricular surface status would allow clinicians to clearly delineate the entire range of information required to visualize and clinically interpret any subtype of LSTV affliction ( Table 1 ). 2
Where does the L5 nerve root come from?
In 1980, McCulloch and Waddell proposed that the functional L5 nerve root always originates from the “last mobile” segment of the spine. The last mobile segment of the spine is defined as the lowest level with a fully formed disc space, bilateral facet joints and two free transverse processes which do not articulate with the ala of the sacrum or the pelvis. Therefore, in the case of a sacralized L5, the functional L5 nerve root corresponds to the anatomical L4 nerve root. In patients with a lumbardized S1, the last fully mobile level is usually L6-S2, and the functional L5 nerve root corresponds with the L6 nerve root. 22 Chang et al. agreed, concluding that neurologic symptoms caused by the L6 nerve root compression resemble those of the L5 rather than the S1 nerve root compression in the normal configuration. 23 In 2008, Kim et al. suggested in the case of lumbardized S1 (L6), the distribution of motor and sensory symptoms caused by the lumbardized S1 (L6) nerve root stimulation is similar to that of the S1 nerve root stimulation in the normal configuration. 24 Furthermore, Hinterdorfer et al. implemented intraoperative electrophysiological monitoring by means of evoked EMG to compare segmental innervation in patients with 5LVB and 6LVB. This study provides strong evidence that the function of the lumbosacral nerve root is not significantly altered in patients with 6LVB, meaning that the L6 nerve root is equivalent to the S1 nerve root in patients with 5LVB. In addition, the root emerging from L6/S not only primarily resembles the S1 root but also shows characteristics of the S2 nerve, with a tendency to innervate the biceps femoris muscle. 25 Seyfert, with careful use of cremasteric reflex, concluded that lumbarization shows a dermatome gap between the lumbar dermatomes C1-C3 and the sacral dermatomes S2 and S3, which lay significantly more ventral than in patients with a normal spinal configuration. 26 The alteration in nerve root innervation caused by a transitional vertebra may make it difficult to find the pain generator. Therefore, in patients receiving epidurals or selective nerve root blocks, one should be aware of a transitional segment before initiating the injection. 24
Which type of transitional disc is smaller than type 1?
A Type 2 transitional disc is smaller than Type 1, maintains its signal intensity, lacks an intra-nuclear cleft, shows evidence of anterior endplate fusion and concave endplates to the disc and is associated with the complete fusion of the LSTV to the sacrum. 56.
Is LSTV a common finding?
Conclusions Due to the common finding of low back pain and the wide prevalence of LSTV in the general population, it is essential to differentiate between symptoms origina ting from an anomalous psu edoarticulation from other potential sources of low back pain. Further studies with larger sample sizes and longer follow-up time would better demonstrate the effectiveness of surgical resection and help guide treatment.
Which modality is most reliable to diagnose far out entrapment of the L5 nerve root?
The authors emphasized that selective radiculography is the most reliable modality to diagnose far-out entrapment of the L5 nerve root and that CT in combination with radiculography clearly demonstrates not only the degree of L5 nerve root impingement, but also the etiology of the L5 nerve root compression. 80.
What is the name of the irregularity of the spine where the fifth vertebra is fused to the sacrum bone?
Sacralization is a common irregularity of the spine, where the fifth vertebra is fused to the sacrum bone at the bottom of the spine. The fifth lumbar vertebra, known as L5, may fuse fully or partially on either side of the sacrum, or on both sides. Sacralization is a congenital anomaly that occurs in the embryo.
Which vertebrae are used for electric denervation?
A 2015 study reported on the use of electric denervation as a minimally invasive method for pain relief in the space between the 5th lumbar vertebra and the sacrum.
What percentage of sacralization is in the general population?
Estimates of the incidence of sacralization in the general population vary widely, from 4 to 36 percent . The wide range of estimates is attributed#N#Trusted Source#N#to differences of diagnostic methods and definition.
What are the symptoms of sacralization?
Other symptoms associated with sacralization may include: arthritis at the fusion site. bursitis. disc degeneration. biomechanical difficulties in movement. limits to range of motion. posture control problems. scoliosis.
When does sacralization occur?
The cause of sacralization isn’t yet known. It occurs during embryonic development, when the vertebrae begin to ossify, in about the eighth week.
When was sacralization first described?
The association between sacralization and lower back pain was first described in 1917. Trusted Source. by the Italian physician Mario Bertolotti, and was called “Bertolotti’s Syndrome.”. The question of pain causality has been a subject of debate in the medical literature ever since.
Is sacralization a congenital disorder?
Sacralization is a common congenital abnormality that often has no symptoms. Whether or not it causes back pain has been a subject of debate since sacralization was first described. If you have pain symptoms, conservative and surgical treatments are available. Last medically reviewed on March 20, 2018.