What foods should you eat while recovering from pancreatitis?
Hemorrhagic pancreatitis is a rapid progression of acute pancreatitis with rupture of pancreatic vessels and subsequent hemorrhage (see Table 12-4). In hemorrhagic pancreatitis, there is diffuse enzymatic destruction of the pancreatic substance caused by a sudden escape of active pancreatic enzymes into the glandular parenchyma (Figure 12-32). These enzymes cause focal …
What is the best remedy for pancreatitis?
Translocation of large volumes of albumin-rich fluid from the intravascular compartment to the retroperitoneum and pleural and abdominal cavities is in part responsible for many of the …
How to lower your risk of future pancreatitis attacks?
· Sixty percent of all acute haemorrhage in the presence of pancreatitis occurs as the result of ruptured pseudo-aneurysms in the presence of necrotising pancreatitis. …
Can chronic pancreatitis be cured completely?
· a) Major haemorrhage: as defined by an acute reduction in haemoglobin concentration of at least 2 g/dl in a patient with overt bleeding and/or hemodynamic instability …
What is pancreatic hemorrhage?
Hemorrhagic pancreatitis is characterized by bleeding within or around the pancreas, and is usually considered a late sequela of acute pancreatitis.
How common is hemorrhagic pancreatitis?
Introduction: Acute pancreatitis (AP) is an uncommon disease with a wide clinical course varying from mild and self-limiting to severe with eventual death. However, death caused by AP is rare. Most cases of AP reported in the English-language literature are based on clinical data; few are medico-legal studies.
What enzyme causes hemorrhagic pancreatitis?
Three enzymes derived from pancreatic acinar cells—amylase, lipase, and the proenzyme trypsinogen—have been tested as biochemical markers of acute pancreatitis; serum amylase is the most commonly used of these in clinical practice.
What are the symptoms of hemorrhagic pancreatitis?
SymptomsUpper abdominal pain.Abdominal pain that radiates to your back.Tenderness when touching the abdomen.Fever.Rapid pulse.Nausea.Vomiting.
How is hemorrhagic pancreatitis treated?
Transcatheter arterial embolization (TAE) is increasingly used as the first-line treatment for hemorrhage complicating pancreatitis and post-pancreatectomy.
How is hemorrhagic pancreatitis diagnosed?
To diagnose acute pancreatitis, your doctor tests your blood to measure two digestive enzymes: amylase and lipase. High levels of these two enzymes mean you probably have acute pancreatitis. They'll also test your blood for white blood cells, blood sugar, calcium, and liver function.
How can acute hemorrhagic pancreatitis be prevented?
These include:Maintain a healthy lifestyle or lose weight, if needed. By keeping your body at a healthy weight, you can make your pancreas work better and reduce some risk factors for pancreatitis. ... Avoid alcohol. Heavy alcohol use is one of the leading causes of both acute and chronic pancreatitis. ... Don't smoke.
What is acute hemorrhage pancreatitis?
Acute hemorrhagic pancreatitis is an inflammation of the pancreas. It often occurs suddenly and quickly, and in some cases, could be fatal. So, what is it exactly? Acute pancreatitis occurs when the pancreas unexpectedly becomes swollen.
What causes a pancreas to be a duct?
genetic disorders of your pancreas. Other causes include. blockage in your pancreatic duct. high levels of blood fats, called lipids. high level of calcium in your blood. In many cases, doctors can’t find the cause of pancreatitis. This is called idiopathic pancreatitis.
What are the symptoms of pancreatitis?
fast heartbeat. swollen or tender abdomen. People with acute pancreatitis usually look and feel seriously ill and need to see a doctor right away. The main symptom of pancreatitis is pain in your upper abdomen that may spread to your back.
What is it called when you have a gallstone in your pancreas?
Gallstones cause inflammation of your pancreas as stones pass through and get stuck in a bile or pancreatic duct. This condition is called gallstone pancreatitis.
How long does pancreatitis last?
begins slowly or suddenly in your upper abdomen. sometimes spreads to your back. can be mild or severe. may last for several days. Other symptoms may include. fever. nausea and vomiting. fast heartbeat.
How to know if pancreatitis is getting worse?
Seek care right away for pancreatitis. Seek care right away for the following symptoms of severe pancreatitis: pain or tenderness in the abdomen that is severe or becomes worse. nausea and vomiting. fever or chills. fast heartbeat. shortness of breath. yellowish color of the skin or whites of the eyes, called jaundice.
Does pancreatitis hurt when you eat?
Most people with chronic pancreatitis. feel pain in the upper abdomen, although some people have no pain at all. The pain may. spread to your back. become constant and severe. become worse after eating. go away as your condition gets worse.
Can pancreatitis cause pain?
People with acute or chronic pancreatitis may feel the pain in different ways.
What are the risk factors for pancreatitis?
Other risk factors include ingestion of a high-fat meal, endocrine disease (hyperglucocorticoidism or hypothyroidism), hypercalcemia, uremia, trauma, or treatment with the immunosuppressive drug, azathioprine. Damage or disease of the biliary tree or obstructions of the pancreatic duct may cause pancreatitis.
What is the pathogenesis of acute pancreatitis?
The pathogenesis of acute pancreatitis is complex and includes the intra-acinar activation of digestive enzymes resulting in degeneration and necrosis of acinar cells, leading to autodigestion of the pancreatic parenchyma and an intense concurrent inflammatory response.
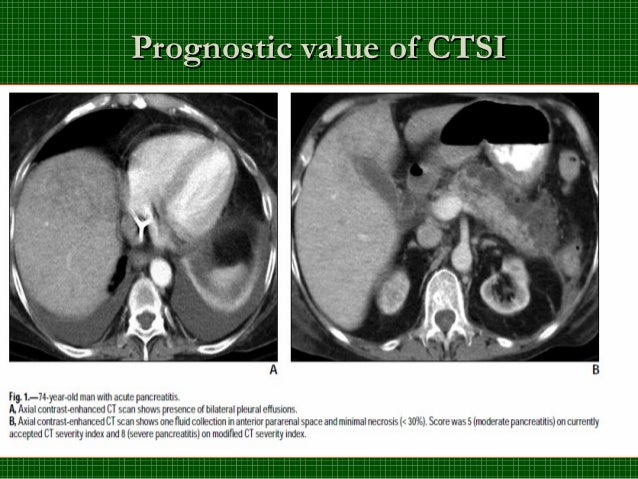
What is the axial ECT of necrotizing and hemorrhagic pancreatitis complicated
Axial CECT of necrotizing and hemorrhagic pancreatitis complicated by infection shows extensive pancreatic necrosis with an air-fluid level , indicating a gas-forming infection.
How to treat acute necrotizing pancreatitis?
Initially, severe acute pancreatitis is characterized by SIRS. Early management is nonsurgical and solely supportive. Apart from ERCP and sphincterotomy in patients with biliary pancreatitis, no specific treatment regimen exists. In cases of necrotizing disease, prophylactic antibiotics should be used to reduce late septic complications. Several interventional regimens, including fine-needle aspiration, percutaneous or endoscopic drainage of peripancreatic fluid collections and pseudocysts, selective angiography, and catheter-directed embolization of acute pancreatitis–associated bleeding complications, have been well established as diagnostic and therapeutic standards in the management of acute pancreatitis.
What is the term for the destruction of pancreatic tissue?
Acute hemorrhagic pancreatitis is an acute inflammatory process caused by enzyme-mediated destruction of pancreatic and peripancreatic tissue.
How long does pancreatitis last?
Acute pancreatitis typically runs a biphasic course. The first phase is characterized by a systemic inflammatory response syndrome (SIRS) and lasts about 2 weeks. The second phase is characterized by a counteractive antiinflammatory response syndrome (CARS), characterized by a state of immunosuppression. Organ failure in the SIRS phase is considered not to be related to infection but rather to severe systemic inflammation. Organ failure in the CARS phase is related to secondary infections, such as infected necrosis. Infections, however, do occur in the SIRS phase, but bacteremia and (ventilator-associated) pneumonia are the most prominent types. This was found in a large series of acute pancreatitis patients where it was demonstrated that these infections were most often diagnosed in the first week of admission. 4
What are the consequences of pancreatitis?
A recently identified consequence of pancreatitis is damage to the intestinal mucosal barrier leading to translocation of gut microbes across the mucosa, resulting in sepsis and multiple organ failure. Pancreatitis may also predispose patients to the formation of thrombosis of splenic and portal veins. These complications are important causes of mortality among patients with acute pancreatitis.
Why are hemorrhagic fluid collections more evident on MRI than CT?
T2: low-signal intensity hemosiderin rim. Signal abnormalities due to hemorrhage remain visible longer on MRI than on CT.
Does acute hemorrhage have high attenuation?
Acute hemorrhage typically has high attenuation on unen hanced CT scans. The attenuation value then decreases as the hematoma ages through time 5.
Is hemorrhagic pancreatitis a sequela?
Hemorrhagic pancreatitis is characterized by bleeding within or around the pancreas, and is usually considered a late sequela of acute pancreatitis.
What is the most important thing to do for a patient with hemorrhagic pancreatitis
Adequate initial resuscitation and intensive follow-up are probably the most important elements in the management of patients with hemorrhagic pancreatitis. Careful monitoring of fluid and electrolytes and blood gases is required to avoid shock and renal and pulmonary failure.
How many patients survived hemorrhagic pancreatitis?
An experience with 68 patients with hemorrhagic pancreatitis identified at operation or autopsy is reported. Sixteen of the patients were subjected to operation, and 6 survived after celiotomy and peritoneal irrigation. There were no survivors in the unoperated group. Death when the pancreas is hemo …
How many patients with pancreatitis survive?
An experience with 68 patients with hemorrhagic pancreatitis identified at operation or autopsy is reported. Sixteen of the patients were subjected to operation, and 6 survived after celiotomy and peritoneal irrigation. There were no survivors in the unoperated group. Death when the pancreas is hemorrhagic and due to pancreatitis occurs an average of 10 days after the onset of symptoms or within 7 days of hospitalization. In eight patients who presented in coma, the diagnosis was not established before death. Early recognition of patients with hemorrhagic pancreatitis can be facilitated by the routine use of amylase and methemalbumin determinations and peritoneal lavage. Translocation of large volumes of albumin-rich fluid from the intravascular compartment to the retroperitoneum and pleural and abdominal cavities is in part responsible for many of the signs, symptoms, and complications of hemorrhagic pancreatitis. These include hemoconcentration, hypotension, tachycardia, tachypnea, ascites, abdominal distress, respiratory insufficiency, and renal failure. Adequate initial resuscitation and intensive follow-up are probably the most important elements in the management of patients with hemorrhagic pancreatitis. Careful monitoring of fluid and electrolytes and blood gases is required to avoid shock and renal and pulmonary failure. The need for careful monitoring is emphasized by the number of our patients in whom inadequacies of fluid replacement and ventilation were often not appreciated until the patient was in extremis from shock or respiratory or renal failure. Antibiotics are indicated in patients with biliary tract disease and penetrating ulcer in whom the risk of secondary infection is considerable. Associated diseases that initiated pancreatitis and that in themselves may be life-threatening, such as acute cholecystitis or cholangitis, should be promptly treated by operation. Diagnostic and therapeutic lavage are justified in the treatment of hemorrhagic pancreatitis. Resection of the necrotic pancreas should be considered when the patient fails to improve after lavage and nonoperative resuscitation.
How long does it take to die from pancreatitis?
Death when the pancreas is hemorrhagic and due to pancreatitis occurs an average of 10 days after the onset of symptoms or within 7 days of hospitalization. In eight patients who presented in coma, the diagnosis was not established before death.
Is lavage necessary for pancreatitis?
Associated diseases that initiated pancreatitis and that in themselves may be life-threatening, such as acute cholecystitis or cholangitis, should be promptly treated by operation. Diagnostic and therapeutic lavage are justified in the treatment of hemorrhagic pancreatitis.
What is the name of the inflammation of the pancreas that causes the death of the pancreas?
Acute Hemorrhagic Pancreatitis Symptoms. Acute hemorrhagic pancreatitis is the sudden inflammation of the pancreas 1. This leads to death of pancreatic tissue and the formation of lesions, causing extensive bleeding. The pancreas is a digestive organ behind the stomach that secretes essential enzymes needed for the digestion of certain foods, ...
Where does pancreatitis pain spread?
In severe cases, the pain can spread to the side, back or lower left shoulder. One of the hallmark symptoms of acute hemorrhagic pancreatitis is abdominal pain--particularly in the area of the pancreas, the upper middle or left side of the abdomen, explains MedlinePlus 1.
How to tell if you have pancreatitis?
One of the hallmark symptoms of acute hemorrhagic pancreatitis is abdominal pain--particularly in the area of the pancreas, the upper middle or left side of the abdomen, explains MedlinePlus 1. The pain often increases in severity, turning into a constant pain that lasts for several days. The pain often worsens in the few minutes after eating or drinking--especially if the meal contains high amounts of fat or is accompanied by large amounts of alcohol, explains an article published in the July 2000 issue of American Family Physician. Lying down flat on the back often makes the pain worse. In severe cases, the pain can spread to the side, back or lower left shoulder.
Can pancreatitis cause vomiting?
An episode of acute hemorrhagic pancreatitis often causes severe flu-like symptoms 1. Nausea and vomiting are frequent symptoms, occurring in approximately 85 percent of patients with acute hemorrhagic pancreatitis, according to the Johns Hopkins Department of Gastroenterology and Hepatology 1 2. A person may also experience a high fever, accompanied by sweating, a take on a generally ill-looking appearance.
Does pancreatitis cause hiccups?
In people with acute hemorrhagic pancreatitis, the pancreas does not produce enough digestive enzymes 1. This can have a variety of effects on the digestive system. The patient may develop clay-colored stools, reports MedlinePlus. Hiccups and indigestion are also frequent symptoms.
Can pancreatitis cause kidney failure?
More severe symptoms may also develop in a person with acute hemorrhagic pancreatitis--including confusion, difficulty breathing, respiratory failure or coma, the John Hopkins Department of Gastroenterology and Hepatology explains 1 2. Kidney failure can also result from acute hemorrhagic pancreatitis, which may require kidney dialysis, according to the Medical University of South Caroline Digestive Disease Center 1. The hemorrhaging pancreas can also leak harsh digestive enzymes into the bloodstream or body cavity, which can damage other internal organs such as the heart and lungs.