What is the most effective birth control?
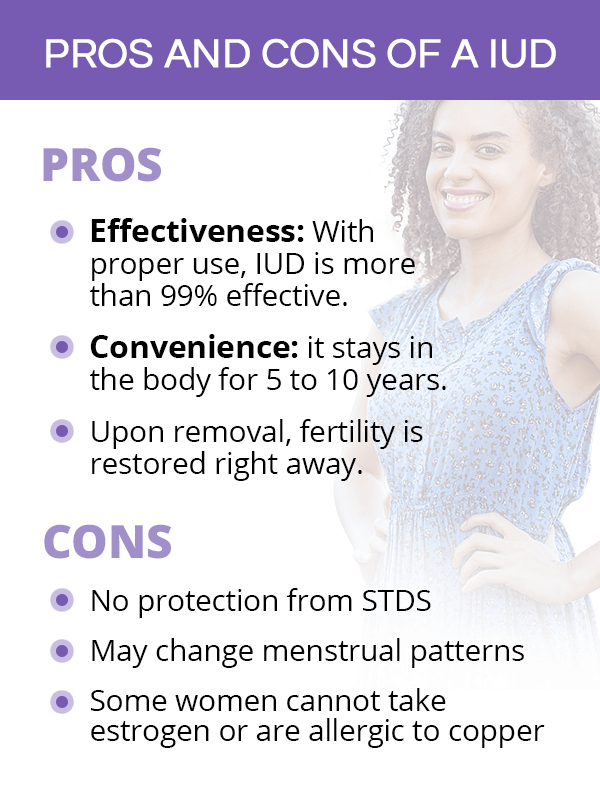
Option #1: IUD. Intrauterine devices (IUDs) are more than 99 percent effective, making them the most effective birth control on the market. IUDs are a form of long-acting reversible contraception (LARC). There are two different types of IUDs available, hormonal and non-hormonal. Both are available by prescription only.
How long after delivery can you breastfeed?
Breastfeeding reduces your chances of becoming pregnant only if you are exclusively breastfeeding. And this method is only reliable for six months after the delivery of your baby. For it to work, you must feed your baby at least every four hours during the day, every six hours at night, and offer no supplement.
Why does a diaphragm fit over the cervix?
It fits over your cervix to prevent sperm from reaching your uterus. A healthcare provider will need to fit you for a diaphragm, and refit after childbirth as the cervix changes and it may no longer fit. This method is about 60 percent effective for women who have already given birth.
How long does Mirena protect you?
The hormone thickens your cervical mucus to prevent sperm from reaching your uterus. Options include: Mirena: provides up to 5 years of protection. Skyla: provides up to 3 years of protection. Liletta: provides up to 3 years of protection. Kyleena: provides up to 5 years of protection.
Is a mini pill safe for breastfeeding?
If you’d like to use an oral contraceptive, the mini-pill is an option. This pill contains progestin only, so it’s considered to be safer for breastfeeding mothers. The pill is typically only available by prescription, but may be found over the counter (OTC) in some states.
When can I start taking progesterone?
Like with many other progestin-containing contraceptives, you can start taking the mini-pill between six and eight weeks after you deliver your baby. It’s between 87 and 99.7 percent effective at preventing pregnancy.
Can you take the morning after pill while breastfeeding?
If you find yourself in a situation where you think your birth control has failed, it’ s safe to use the morning-after pill while breastfeeding. This pill should only be used as a last resort and not as a regular form of birth control. It is available OTC or at a reduced cost by prescription.
What is the most effective form of birth control?
Intrauterine devices (IUDs) are the most effective form of birth control. They can be hormonal or nonhormonal. Both require a prescription.
What are the two types of birth control pills?
There are two types of birth control pills: combination and progestin-only pills. Combination pills are daily pills that contain both estrogen and progestin, and they are the most common type of birth control pills. However, they are not generally recommended postpartum because they contain estrogen, which can lower milk supply.
Why is birth control important?
Birth control plays an integral part in family planning. Knowing your contraceptive options while breastfeeding gives you the power to make the right choice for yourself and your family. Taking time between pregnancies is important for maternal and child health.
What is the time between giving birth and getting pregnant again called?
The time between giving birth and getting pregnant again is called birth spacing, pregnancy spacing, and interpregnancy interval (also called IPI). It should be noted that birth spacing of more than five years is associated with its own risks, such as an increased chance of preeclampsia, a serious pregnancy complication defined by high blood pressure and signs of damage to another organ system, usually the liver or kidneys. 3
How long after giving birth can you start using estrogen?
For the first three weeks after giving birth, you should not use a method that has the hormone estrogen, like the pill, patch, or ring. 1 After three weeks , you can start any of these methods.
Is it safe to take birth control while breastfeeding?
Overall, birth control is safe while breastfeeding and won't impact the health of you or your baby. 1 Many contraceptives can be started immediately after giving birth, including intrauterine devices (IUDs), arm implants, birth control shots, and progestin-only pills.
Is there estrogen in birth control?
Given the risks associated with estrogen contraceptives, progestin-only birth control options are preferred. 4 Hormonal birth control that contains estrogen can include the pill, NuvaRing, and a skin patch.
What are non-hormonal birth control options?
Other non-hormonal birth control options are condoms, internal condoms, diaphragm, and cervical cap.
How long after birth can you use birth control?
You can use our birth control app to keep track of your insertion date and removal date. For the first 3 weeks after giving birth, don’t use a method that has the hormone estrogen, like the pill, patch, or ring. After 3 weeks, you can start any of these methods.
What non-hormonal methods can I use?
You can safely use non-hormonal birth control while breast feeding. For up to the first 6 months after your baby is born, you can rely on breastfeeding as birth control if you have not gotten your period yet and are not feeding your baby formula or food.
Can you put a cap in your vagina?
If you used a diaphragm or cervical cap in the past, wait until your first postpartum checkup to begin using that method again. Most doctors recommend that you don’t put anything in your vagina until that first checkup. You may also need a new size.
Can you use birth control pills after giving birth?
Yes, if you’re breastfeeding, you can safely use hormonal methods. They won’t hurt you or your baby. You can start using the shot, implant, Skyla and Mirena IUDs, and some types of birth control pills (called mini-pills) right after giving birth.
Recommended Birth Control Options
Because estrogen can affect a mother’s milk supply, doctors generally recommend using progestin-based contraceptives or barrier methods. However, based on physician discretion, an estrogen-based contraceptive may be recommended.
Progestin-Only Contraceptives
When started at least six weeks after delivery, contraceptives that contain only progestin are recommended for mothers who breastfeed. This hormone typically does not affect a woman’s ability to produce breast milk.
Non-Hormonal Contraception
These methods don’t use any forms of hormones, are safe, and won’t affect your ability to produce milk.
When to start progesterone after delivery?
When started at least six weeks after delivery, contraceptives that contain only progestin are recommended for mothers who breastfeed. This hormone typically does not affect a woman’s ability to produce breast milk.
Is it important to choose the right method of birth control?
Congratulations on the birth of your baby! The miracle of birth is extremely rewarding, but many moms choose to wait a while before experiencing the nine-month process again. For moms who want to breastfeed their child, it is important to choose the right method of birth control.
Can you breastfeed with estrogen?
The most important thing to remember is to avoid birth control pills that contain estrogen . Studies have found that birth control containing estrogen lowers milk supply and shortens the amount of time you can breastfeed.
Is barrier contraception safe?
Barrier methods of contraception are the more traditional forms of birth control. Since these methods don’t use any forms of hormones, it is natural, safe, and won’t affect your ability to produce milk.
Avoid Estrogen-Based Contraceptives
The most important thing to remember is to avoid birth control pills that contain estrogen . Studies have found that birth control containing estrogen lowers milk supply and shortens the amount of time you can breastfeed.
Recommended Birth Control Options
Because of the negative effects of estrogen on a mother’s milk supply, doctors recommend using progestin-based contraceptives or barrier methods.
Progestin-Only Contraceptives
When started at least six weeks after delivery, contraceptives that contain only progestin are recommended for mothers who breastfeed. This hormone typically does not affect a woman’s ability to produce breast milk.