
Symptoms
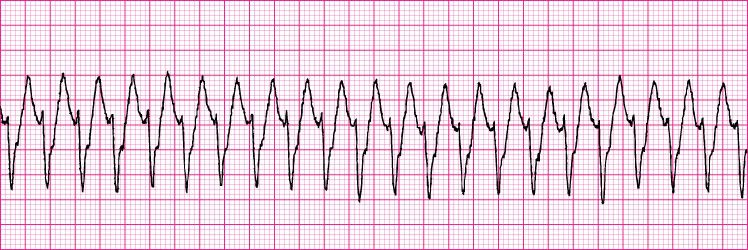
VTACH + VFIB | A Nurse’s Guide to Ventricular Arrhythmias
- Check for a Pulse / Breathing. If you see a ventricular arrhythmia on the monitor, you should immediately assess your patient first.
- Call an RRT or Code Blue. If the patient is pulseless, call for help and call a CODE BLUE. ...
- Start CPR if Needed. ...
- Give Life-Saving Treatment. ...
- Reverse any known causes (Hs & Ts) In ACLS you are taught all about Hs and Ts. ...
Causes
Ventricular tachycardia is an important cause of sudden death. The risk and consequently the therapeutic approach are determined by the underlying heart disease. Ventricular tachycardia is most commonly associated with ischemic heart disease or other forms of structural heart disease that are associated with a risk of sudden death.
Complications
There are some treatment options for patients with ventricular tachycardia, according to Johns Hopkins Medicine. One option is a radiofrequency ablation, a procedure that destroys the cells that can cause the condition. It is less effective, however, in people with structural heart disease.
How do you treat V tach?
Ventricular tachycardia is a heart rhythm disorder that is caused by abnormal electrical signals in the lower chambers of the heart. Also called VT or V-tach, ventricular tachycardia may last only for a few seconds but can also last for minutes at a time, in which case it can be life-threatening.
What is Vtach and risk?
What to do for V tach?
What causes V tach?
What MED do you push for Vtach?
Intravenous Push/IO: 1mg epinephrine IV is given every 3-5 minutes.
Do you shock V tach with a pulse?
Ventricular tachycardia is a poorly perfusing rhythm; patients may present with or without a pulse. Most patients with this rhythm are unconscious and pulseless and defibrillation is needed to “reset” the heart so that the primary pacemaker (usually the Sinoatrial Node) can take over.
What do you do for Vtach without a pulse?
Medical treatment of pulseless VT usually is carried out along with defibrillation and includes intravenous vasopressors and antiarrhythmic drugs. 1 mg of epinephrine IV should be given every 3 to 5 minutes. Epinephrine can be replaced by vasopressin given 40 units IV once.
How is Vtach Nursing treated?
Patients with pulseless ventricular tachycardia are treated the same as those with ventricular fibrillation, meaning they require immediate cardiopulmonary resuscitation (CPR) and defibrillation. Once the rhythm converts, the patient will need an infusion of amiodarone or lidocaine.
What are the 3 shockable rhythms?
VF and pulseless VT are shockable rhythms and treated in similar fashion. Asystole and PEA are also included in the cardiac arrest algorithm but are non-shockable rhythms. Ventricular fibrillation and pulseless ventricular tachycardia are treated using the left branch of the cardiac arrest arrest algorithm.
Is V-tach always pulseless?
Ventricular tachycardia is not always pulseless. In ventricular tachycardia, the heart rate usually exceeds 100 beats per minute. A normal resting heart rate is 60 to 100 beats per minute.
Do you give epinephrine in V-tach?
Currently, the ACLS protocol for v fib and pulseless v tach recommends that epinephrine be given after the second defibrillation. Many hospitals and EMS systems, however, have been giving it earlier.
What do you do for V-tach ACLS?
Apply defibrillator pads (or paddles) and shock the patient with 120-200 Joules on a biphasic defibrillator or 360 Joules using a monophasic. Continue High Quality CPR for 2 minutes (while others are attempting to establish IV or IO access).
How do you respond to V-tach?
In a pulseless patient, begin immediate CPR and attach AED or external defibrillator. If Vtach or Vfib, prepare for defibrillation. If pulse is present, attach EKG or defibrillator and evaluate rhythm. If patient is unstable and not polymorphic Vtach, prepare for synchronized cardoversion.
What happens during V-tach?
What is ventricular tachycardia? Ventricular tachycardia (VT or V-tach) is a type of abnormal heart rhythm, or arrhythmia. It occurs when the lower chamber of the heart beats too fast to pump well and the body doesn't receive enough oxygenated blood.
Do you call code blue for V-tach with a pulse?
Call an RRT or Code Blue If the patient is pulseless, call for help and call a CODE BLUE. If the patient has a pulse but in VTACH, an RRT should be called as this is still an emergent rhythm and the patient can go down at any minute.
What rhythms can you shock?
The two shockable rhythms are ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) while the non–shockable rhythms include sinus rhythm (SR), supraventricular tachycardia (SVT), premature ventricualr contraction (PVC), atrial fibrilation (AF) and so on.
When should you avoid synchronized shock?
The T wave is considered the vulnerable period, especially the middle and second half of the T wave. By timing the shock to be delivered during the QRS complex, electrical stimulation is avoided during the vulnerable period, which reduces the risk of inducing ventricular fibrillation.
Do you shock VFIB?
Ventricular fibrillation is life-threatening and requires prompt treatment. Collapse and sudden cardiac death will follow in minutes unless medical help is provided immediately. If treated in time, ventricular fibrillation can be converted into a normal rhythm by shocking the heart with a device called a defibrillator.
How many beats is considered V-tach?
Ventricular tachycardia (VT) is a fast, abnormal heart rhythm (arrhythmia). It starts in your heart's lower chambers, called the ventricles. VT is defined as 3 or more heartbeats in a row, at a rate of more than 100 beats a minute.
Overview
Symptoms
Causes
Risk Factors
Complications
Prevention
- When the heart beats too fast, it may not pump enough blood to the rest of the body. So the organs and tissues may not get enough oxygen. Signs and symptoms that occur during an episode of ventricular tachycardia are due to a lack of oxygen and may include: 1. Chest pain (angina) 2. Dizziness 3. Pounding heartbeat (palpitations) 4. Lightheadedness 5. Shortness of br…
Diagnosis
- Ventricular tachycardia is caused by faulty heart signaling that triggers a fast heart rate in the lower heart chambers (ventricles). The fast heart rate doesn't allow the ventricles to fill and squeeze (contract) to pump enough blood to the body. Many things can cause or contribute to problems with heart signaling and lead to ventricular tachycardia. These include: 1. Prior heart at…
Treatment
- Any condition that puts a strain on the heart or damages heart tissue can increase the risk of ventricular tachycardia. Lifestyle changes or proper medical treatment for the following conditions and events may lower the risk: 1. Heart disease 2. Medication side effects 3. Severe electrolyte imbalances 4. Use of stimulant drugs such as cocaine or methamphetamine A family history of t…
Clinical Trials
- Complications of ventricular tachycardia depend on: 1. How fast the heart is beating 2. How long the rapid heart rate lasts 3. Whether there are other heart conditions Possible complications of ventricular tachycardia include: 1. Frequent fainting spells or unconsciousness 2. Heart failure 3. Sudden death caused by cardiac arrest
Coping and Support
- The best ways to prevent tachycardia are to maintain a healthy heart and prevent heart disease. If you already have heart disease, monitor it and follow your treatment plan. Be sure you understand your treatment plan, and take all medications as prescribed. Take the following steps to keep the heart healthy: 1. Eat a balanced, nutritious diet.A die...
Preparing For Your Appointment