
Glucose Uptake PGUA (mg/min/kgmuscle) is the active muscle peripheral glucose uptake rate and PAMM is the percentage of active muscle mass, taking the basal PGU equal to 35mg/min and the skeletal muscle mass approximately equal to 28kg in an average 70kg weighted human. From: Personalized Predictive Modeling in Type 1 Diabetes, 2018
Full Answer
How does exercise increase glucose uptake?
Intracellular glucose metabolism
- Glycogen content. During exercise, muscle preferentially utilizes glycogen stores to provide glucose for ATP generation; therefore, the rate of muscle glucose uptake from the blood is inversely related to muscle ...
- Intracellular phosphorylation of glucose. ...
- Glycolysis. ...
Does glucose uptake in muscles without insulin?
Working skeletal muscle: Insulin is not required for uptake of glucose in working skeletal muscle because exercise mobilizes GLUT4 in skeletal muscle. People Also Asked, Do muscles need insulin to use glucose? Likewise, people ask, do muscles need insulin to use glucose?
What is important in glucose metabolism?
Vitamin D may improve glucose metabolism by stimulating insulin secretion from pancreatic beta cells and by improving peripheral insulin sensitivity.
What is the average glucose count?
What is considered a normal blood sugar level? The normal blood sugar (glucose) level for a healthy adult (without diabetes) should be less than 126 mg/dL (milligrams per deciliter) or 6 mmol/L (millimole per litre) before fasting and meals, and below 200mg/dL (or 11 mmol/L) two hours after meals.
Glucose Uptake
Method of glucose uptake differs throughout tissues depending on two factors; the metabolic needs of the tissue and availability of glucose.
Glucose Uptake Mediated By Glucose Transporter 1 Is Essential For Early Toothmorphogenesis And Size Determination Of Murine Molars
1. Dev Biol. 2012 Mar 1;363 (1):52-61. doi: 10.1016/j.ydbio.2011.12.020. Epub 2011Dec 20. Glucose uptake mediated by glucose transporter 1 is essential for early toothmorphogenesis and size determination of murine molars. Ida-Yonemochi H (1), Nakatomi M, Harada H, Takata H, Baba O, Ohshima H.
Glucose Transporters In Cardiac Metabolism And Hypertrophy
Glucose Transporters in Cardiac Metabolism and Hypertrophy 1Mitochondria and Metabolism Center, University of Washington, Seattle, Washington, USA The publisher's final edited version of this article is available at Compr Physiol See other articles in PMC that cite the published article.
Glucose Transport
The oxidation of glucose represents a major source of metabolic energy for mammalian cells. Because the plasma membrane is impermeable to polar molecules such as glucose, the cellular uptake of this important nutrient is accomplished by special carrier proteins called glucose transporters [1] [2] [3] [4] [5] [6] [7].
Pdb-101: Glucose Transporters
Glucose transporters deliver glucose molecules one-by-one across cell membranes. GLUT3 is shown on the left in the open outward conformation, and GLUT1 is shown on the right in an open inward conformation. Glucose is the fuel that powers most of the biosphere.
Increased Muscle Glucose Uptake After Exercise: No Need For Insulin During Exercise
It has recently been shown that insulin sensitivity of skeletal muscle glucose uptake and glycogen synthesis is increased after a single exercise session. The present study was designed to determine whether insulin is necessary during exercise for development of these changes found after exercise.
The Molecular Basis Of Insulin-stimulated Glucose Uptake: Signalling, Trafficking And Potential Drug Targets
Abstract The search for the underlying mechanism through which insulin regulates glucose uptake into peripheral tissues has unveiled a highly intricate network of molecules that function in concert to elicit the redistribution or ‘translocation’ of the glucose transporter isoform GLUT4 from intracellular membranes to the cell surface.
What are the two ways in which glucose uptake can take place?
The two ways in which glucose uptake can take place are facilitated diffusion (a passive process) and secondary active transport (an active process which on the ion-gradient which is established through the hydrolysis of ATP, known as primary active transport ).
Where does glucose go in the kidney?
However, in the kidney, glucose is reabsorbed from the filtrate in the tubule lumen, where it is at a relatively low concentration, passes through the simple cuboidal epithelia lining the kidney tubule, and into the bloodstream where glucose is at a comparatively high concentration. Therefore, the concentration gradient of glucose opposes its reabsorption, and energy is required for its transport.
How many different types of glucose transporters are there?
There are over 10 different types of glucose transporters; however, the most significant for study are GLUT1-4.
Where is GLUT4 expressed?
During fasting, some GLUT4 transporters will be expressed at the surface of the cell. However, most will be found in cytoplasmic vesicles within the cell. After a meal and at the binding of insulin (released from the islets of Langerhans) to receptors on the cell surface, a signalling cascade begins by activating phosphatidylinositolkinase activity which culminates in the movement of the cytoplasmic vesicles toward the cell surface membrane. Upon reaching the plasmalemma, the vesicles fuse with the membrane, increasing the number of GLUT4 transporters expressed at the cell surface, and hence increasing glucose uptake.
Where is GLUT2 located?
They are located in the plasma membranes of hepatocytes and pancreatic beta cells (in mice, but GLUT1 in human beta cells; see Reference 1). The high Km of GLUT2 allows for glucose sensing; rate of glucose entry is proportional to blood glucose levels.
Do beta cells differ in glucose transporter?
1. De Vos, A., H. Heimberg, et al. (1995). "Human and rat beta cells differ in glucose transporter but not in glucokinase gene expression." The Journal of Clinical Investigation 96 (5): 2489-2495.
Is glucose dependent on sodium?
Hence reabsorption of glucose is dependent upon the existing sodium gradient which is generated through the active functioning of the NaKATPase. As the cotransport of glucose with sodium from the lumen does not directly require ATP hydrolysis but depends upon the action of the ATPase, this is described as secondary active transport.
How does glucose uptake occur?
The two ways in which glucose uptake can take place are facilitated diffusion (a passive process) and secondary active transport (an active process which depends on the ion-gradient which is established through the hydrolysis of ATP, known as primary active transport). Facilitated diffusion There are over 10 different types of glucose transporters; however, the most significant for study are GLUT1-4. GLUT1 and GLUT3 are located in the plasma membrane of cells throughout the body, as they are responsible for maintaining a basal rate of glucose uptake. Basal blood glucose level is approximately 5mM (5 millimolar). The Km value (an indicator of the affinity of the transporter protein for glucose molecules; a low Km value suggests a high affinity) of the GLUT1 and GLUT3 proteins is 1mM; therefore GLUT1 and GLUT3 have a high affinity for glucose and uptake from the bloodstream is constant. GLUT2 in contrast has a high Km value (15-20mM) and therefore a low affinity for glucose. They are located in the plasma membranes of hepatocytes and pancreatic beta cells (in mice, but GLUT1 in human beta cells; see Reference 1). The high Km of GLUT2 allows for glucose sensing; rate of glucose entry is proportional to blood glucose levels. GLUT4 transporters are insulin sensitive, and are found in muscle and adipose tissue. As muscle is a principal storage site for glucose and adipose tissue for triglyceride (into which glucose can be converted for storage), GLUT4 is important in post-prandial uptake of excess glucose from the bloodstream. Moreover, several recent papers show that GLUT 4 is present in the brain also. The drug Metformin phosphor Continue reading >>
What is the pathway that controls glucose uptake?
The first, and widely investigated, is the insulin activated signaling pathway through insulin receptor substrate-1 and phosphatidylinositol 3-kinase. The second is the insulin-independent signaling pathway, which is activated by contractions. Individuals with type 2 diabetes mellitus have reduced insulin-stimulated glucose uptake in skeletal muscle due to the phenomenon of insulin resistance. However, those individuals have normal glucose uptake during exercise. In this context, physical exercise is one of the most important interventions that stimulates glucose uptake by insulin-independent pathways, and the main molecules involved are adenosine monophosphate-activated protein kinase, nitric oxide, bradykinin, AKT, reactive oxygen species and calcium. In this review, our main aims were to highlight the different glucose uptake pathways and to report the effects of physical exercise, diet and drugs on their functioning. Lastly, with the better understanding of these pathways, it would be possible to assess, exactly and molecularly, the importance of physical exercise and diet on glucose homeostasis. Furthermore, it would be possible to assess the action of drugs that might optimize glucose uptake and consequently be an important step in controlling the blood glucose levels in diabetic patients, in addition to being important to clarify some pathways that justify the development of drugs capable of mimicking the contraction pathway. Key words: diabetes; exercise; glucose uptake; diet; hypoglycemic drugs A captação de glicose nos tecidos peri Continue reading >>
What is the problem with insulin?
Statement of the Problem: In diabetes, the bodys response to insulin is impaired, resulting in elevated levels of blood glucose. Peripheral-tissue glucose uptake is an important regulatory point in controlling blood glucose. After a meal, insulin causes most glucose to be quickly taken up by muscle and adipose tissue. This process is carried out by the fusion of storage vesicles containing GLUT4, a glucose transporter, with the cell surface membrane. Failure of this process results in insulin resistance and elevated blood glucose. To prevent hypoglycemia under fasting conditions, GLUT4 on the cell surface is normally kept low by continuous endocytosis. Because AP2- and clathrin-binding sites have been mapped in GLUT4, this basal endocytosis has been thought to be a signaling-independent, passive process. Yet this concept creates a dilemma: how is this process inhibited during insulin stimulation to avoid a futile cycle of endocytosis and cell surface fusion? Methodology & Findings: We recently identified TXNIP (thioredoxin-interacting protein) as a negative regulator of the class I members of the SLC2 family of glucose transporters, which includes GLUT4. We discovered that TXNIP associates with GLUTs and mediates GLUT endocytosis via the clathrin-dependent pathway, effectively reducing glucose influx. Using TXNIP WT and KO mice, we found that the absence of TXNIP results in higher fasting glucose uptake into muscle and adipose tissue. Using tissue cultures, we found that insulin-induced AKT activation leads to TXNIP phosphorylation that disrupts the TXNIP/GLUT4 interaction, acutely inhibiting GLUT4 endocytosis. Conclusion & Significance: Our results indicate that GLUT4 endocytosis is actually a regulatable process, both in fasting and insulin-stimulated states. Togethe Continue reading >>
Is postprandial blood glucose a predictor of cardiovascular events?
Postprandial Blood Glucose Is a Stronger Predictor of Cardiovascular Events Than Fasting Blood Glucose in Type 2 Diabetes Mellitus, Particularly in Women: Lessons from the San Luigi Gonzaga Diabetes Study
Can cells take up glucose without insulin?
Abstract: Despite evidence to the contrary, there is a widespread misconception that cells cannot take up glucose without insulin. It is believed that these starving cells, by their inability to absorb glucose, cause hyperglycemia (high blood sugar). This brief review of the available scientific literature intends simply to show that 1) considerable glucose uptake occurs independently of insulin, 2) that hyperglycemia is not caused by cells unable to import glucose, 3) AND lastly THAT CELLS ARE NOT STARVING DURING HYPERGLYCEMIA. Important: this text discusses the underlying mechanisms of glucose uptake. It has little clinical significance. Diabetics should continue to use insulin as prescribed by their doctor. As a medical student, i’ve been taught that cells need insulin to absorb glucose. Insulin causes a glucose transporter (glut) to rise to the cell surface. This transporter creates a channel for glucose to flow through. There are about 13 different gluts, and the one that needs insulin is glut4 (possibly 12, also). According to the misconception, glut4 is required for glucose uptake, and that is why insulin is necessary. Without insulin, there will be no glut4, and so we’re told that the cell cannot consume glucose, which causes glucose to build up in the blood – hyperglycemia. This is demonstrably false, as many experiments have shown. While insulin does impact absorption by doubling the glucose uptake speed, we’ll see that it is not required. 1 While it is true that glut4 is largely insulin dependent, it has almost a dozen brothers that function quite well without insulin. 2 take, for example, glut1. It’s nearly everywhere in the body, all the time, and it’s as powerful as the glut4. Glut1 is the day-to-day glucose transporter responsible for basal gl Continue reading >>
Why does my glucose level rise?
These include certain foods, like artificial sweeteners and coffee. Other factors like stress can do it, too. If you live with an endocrine or pancreatic condition , had surgery recently , or are experiencing intense physical stress (say, from a sunburn), you may also see your glucose value rise.
What causes high blood glucose?
Experts are still learning about all the factors that can contribute to high blood glucose. With that in mind, these are the main known causes of high blood glucose.
What is high blood glucose (aka “hyperglycemia”)?
To fully understand your blood glucose levels, it’s important to know: a) what values are actually considered high, and b) factors that can cause your elevated reading in the first place.
What are the health problems that can be caused by high blood glucose levels?
Zanini says that untreated high blood glucose can lead to a wide range of health issues—some of the most common being chronic inflammation, heart disease, vision impairment, kidney disease, nerve damage, tooth decay, damaged blood vessels, and periodontal disease.
Why is my blood sugar low?
Low blood sugar, or hypoglycemia, is the result of too little glucose in the bloodstream. Hyperglycemia usually occurs because your body doesn’t produce enough insulin or can’t properly use the available insulin to remove the glucose from the bloodstream.
How many hours a day do you spend on a glucose monitor?
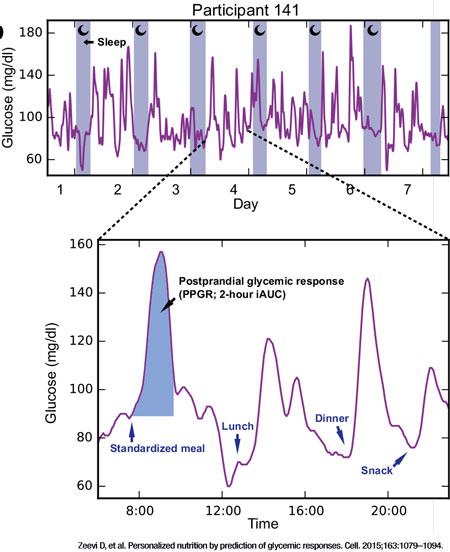
When researchers studied people wearing a continuous glucose monitor who did not have a diabetes diagnosis, they found 93% of individuals reached glucose levels that are considered dangerous, with 10% spending over 2 hours per day in these dangerous levels.
Why is my A1C inaccurate?
Pregnancy, hemoglobin variants, anemia, liver disease, and certain medications can cause inaccurate A1C results. Additionally, the A1C test is measuring your average glucose value over the past 3 months, but averages inherently do not capture highs and lows.
What is a blood glucose test?
A blood glucose test is a blood test that screens for diabetes by measuring the level of glucose (sugar) in a person’s blood.
How does the pancreas respond to the increase in glucose?
The pancreas responds by releasing enough insulin to handle the increased level of glucose — moving the glucose out of the blood and into cells. This helps return the blood glucose level to its former, lower level.
What are the risk factors for diabetes?
The following categories of people are considered "high-risk" candidates for developing diabetes: 1 Individuals who are overweight or obese 2 Individuals who are 45 years of age or older 3 Individuals with first-degree relatives with diabetes (such as parents, children, or siblings) 4 Individuals who are African-American, Alaska Native, American Indian, Asia American, Hispanic/Latino, Native Hawaiian, Pacific Islanders, 5 Women who developed diabetes while they were pregnant or gave birth to large babies (9 pounds or more) 6 Individuals with high blood pressure (140/90 or higher) 7 Individuals with high-density lipoprotein (HDL, the "good cholesterol level") below 25 mg/dl or triglyceride levels at or above 250 mg/dl 8 Individuals who have impaired fasting glucose or impaired glucose tolerance 9 Individuals who are physically inactive; engaging in exercise less than three times a week 10 Individuals who have polycystic ovary syndrome, also called PCOS 11 Individuals who have acanthosis nigricans -- dark, thick and velvety skin around your neck or armpits
What does it mean if your glucose is 100?
If your blood glucose level is 100 to 125 mg/dL (5.6 to 6.9 mmol/L). . . What it means: You have an impaired fasting glucose level (pre-diabetes**) . . . If your blood glucose level is 126 mg/dl (7.0 mmol/L ) or higher on more than one testing occasion. What it means: You have diabetes.
Why is my blood sugar low?
Too low a level of blood sugar, a condition called hypoglycemia, can be caused by the presence of too much insulin or by other hormone disorders or liver disease.
How long do you have to fast for a blood test?
To get an accurate plasma glucose level, you must have fasted (not eaten or had anything to drink except water) for at least 8 hours prior to the test. When you report to the clinic or laboratory, a small sample of blood will be taken from a vein in your arm. According to the practice recommendations of the American Diabetes Association, the results of the blood test are interpreted as follows:
What is the blood pressure of a woman with diabetes?
Women who developed diabetes while they were pregnant or gave birth to large babies (9 pounds or more) Individuals with high blood pressure (140/90 or higher) Individuals with high-density lipoprotein (HDL, the "good cholesterol level") below 25 mg/dl or triglyceride levels at or above 250 mg/dl.
