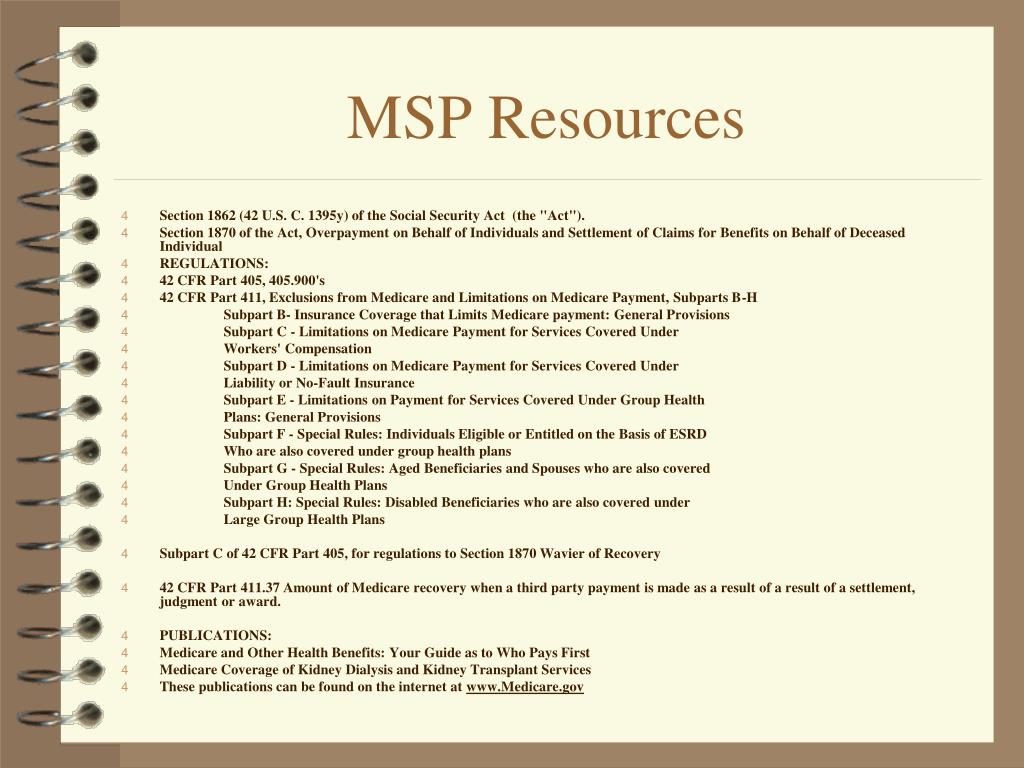
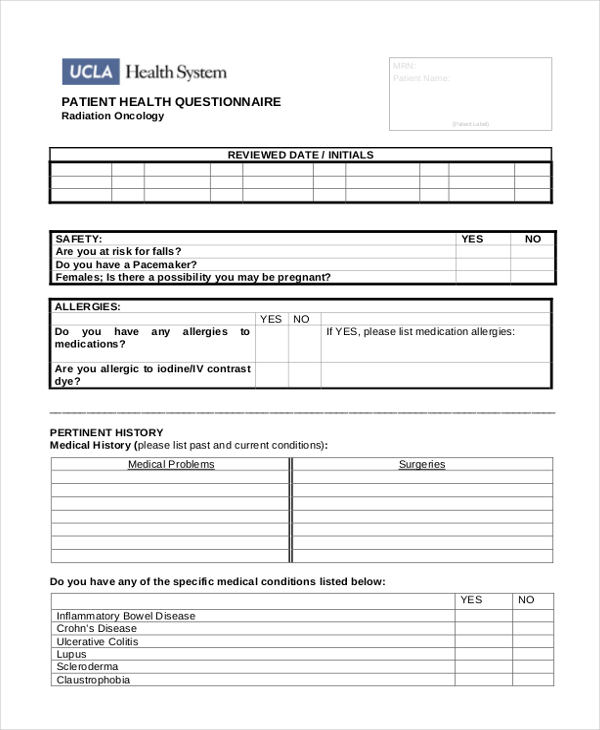
What is an MSP questionnaire? This questionnaire is a model of the type of questions that may be asked to help identify Medicare Secondary Payer (MSP) situations. The instructions will direct the patient to the next appropriate question to determine MSP situations.
How do hospitals use the MSP questionnaire?
Part A Institutional Providers (Hospitals) Use a MSP questionnaire during the admission process. Gather accurate MSP data. Determine if Medicare is the primary payer by asking patients or their representative(s) for MSP information. Bill primary payer before billing Medicare.
What is the Medicare Supplement Program (MSP)?
The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Physicians, non-physician practitioners and suppliers are responsible for gathering MSP data to determine whether Medicare is the primary payer by asking Medicare beneficiaries questions concerning their MSP status.
What are the MSP coverage situations in Minnesota?
Table 1. Common MSP Coverage Situations Medicare Secondary Payer MN Boolet Page 5 of 16 MN006903 April 2021 Individual Condition Pays First Pays Second 65 or older and covered by a Group Health Plan (GHP*) through current employment or spouse’s current employment Entitled to Medicare Employer has less than 20 employees Medicare
How long do I need to keep my MSP questionnaire?
Medicare Secondary Payer Manual, Chapter 3, Section 20 or contact your MAC. Providers must keep completed MSP questionnaire copies and other MSP information for 10 years after the service date. You may keep hard copy files, optical images, microfilms, or microfiches. When storing these files online, keep negative and positive question responses.
What is the purpose of the MSP questionnaire?
The MSP questionnaire is used to determine whether Medicare is the primary or secondary payer. If another insurer is primary, it pays the lion's share of the patient's bill, and Medicare covers the rest.
Is the MSP questionnaire required?
In accordance with guidelines established by the Centers for Medicare & Medicaid Services (CMS), all providers are required to complete the MSP questionnaire upon admission.
What is an MSP form?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.
How often does the MSP questionnaire need to be completed?
once every 90 daysFollowing the initial collection, the MSP information should be verified once every 90 days.
Is MSP questionnaire required for Medicare Advantage plans?
The MSPQ is required for Part A. Providers can check the MSP screen in CWF to ensure the information is accurate before you submit your claim to Medicare.
Will Medicare pay as secondary if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
How do I claim MSP?
Or call us – from the Lower Mainland at 604-683-7151 or from the rest of BC at 1-800-663-7100.
What is a Medicare Secondary Payer questionnaire?
Medicare Secondary Payer Questionnaire. (Short Form) The information contained in this form is used by Medicare to determine if there is other insurance that should pay claims primary to Medicare.
What is MSP code?
Medicare Secondary Payer (MSP) Code.
Does Medicare automatically send claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
What happens when Medicare is secondary?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
How do you know if Medicare is primary or secondary?
If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second . If the employer has fewer than 20 employees and isn't part of a multi-employer or multiple employer group health plan, then Medicare pays first, and the group health plan pays second .
What is a Medicare Secondary Payer questionnaire?
Medicare Secondary Payer Questionnaire. (Short Form) The information contained in this form is used by Medicare to determine if there is other insurance that should pay claims primary to Medicare.
How do I bill Medicare secondary claims electronically?
Electronic Claim Submission of MSP Claims Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
What is MSPQ in epic?
When Sutter implemented the Epic system we decided to create two “Sutter Specific” Medicare Payer Secondary Questionnaire (MSPQ) forms. One for Hospital and one for Foundations and Sutter Community Connect Clients (SCC).
Which of the following is a criterion for a patient to qualify for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
What is the purpose of MSP?
The MSP provisions have protected Medicare Trust Funds by ensuring that Medicare does not pay for items and services that certain health insurance or coverage is primarily responsible for paying. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Is GHP a disability?
Disability and Employer GHP: Individual is disabled, is covered by a GHP through his or her own current employment (or through a family member’s current employment) AND the employer has 100 or more employees (or at least one employer is a multi-employer group that employs 100 or more individuals) GHP pays Primary, Medicare pays secondary.
Is Medicare the primary payer?
Medicare remains the primary payer for beneficiaries who are not covered by other types of health insurance or coverage. Medicare is also the primary payer in certain instances, provided several conditions are met.
What is the MSP questionnaire?
The MSP questionnaire is used to determine whether Medicare is the primary or secondary payer. If another insurer is primary, it pays the lion’s share of the patient’s bill, and Medicare covers the rest.
Is it mandatory to ditch the MSP?
Or hospitals are free to continue to use the MSP questionnaire. Ditching it is not required. Patients will appreciate the end of mandatory questionnaires because sometimes when they return to the hospital the next day or shortly after treatment, they get frustrated at having to answer the same questions again, Gillis says.
Is Medicare a secondary payer?
Hospitals are now free of the Medicare as secondary payer (MSP) questionnaire as long as they do electronic insurance verification and ask patients whether their insurance has changed when they’re admitted as inpatients or register as outpatients. Medicare Transmittal 123, which took effect on Nov.
What is MSP in Medicare?
The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Physicians, non-physician practitioners and suppliers are responsible for gathering MSP data to determine whether Medicare is the primary payer by asking Medicare beneficiaries questions concerning their MSP status.
When sending an MSP claim electronically, should the primary explanation of benefits be sent separately?
When sending an MSP claim electronically, the primary explanation of benefits should not be sent separately.
When Medicare is the secondary payer, what is the primary payer?
When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, ...
Who is responsible for obtaining primary insurance information from the beneficiary and billing Medicare appropriately?
It is the provider' s responsibility to obtain primary insurance information from the beneficiary and bill Medicare appropriately.
How often do you need to collect MSP information?
Following the initial collection, the MSP information should be verified once every 90 days. If the MSP information collected by the hospital, from the beneficiary or his/her representative and used for billing, is no older than 90 calendar days from the date the service was rendered, then that information may be used to bill Medicare for recurring outpatient services furnished by hospitals. This policy, however, will not be a valid defense to Medicare’s right to recover when a mistaken payment situation is later found to exist.
When a provider receives a reduced no fault payment because of failure to file a proper claim, what is?
When a provider receives a reduced no-fault payment because of failure to file a proper claim, (see Chapter 1, §20 for definition), the Medicare secondary payment may not exceed the amount that would have been payable if the no-fault insurer had paid on the basis of a proper claim.
Is GHP primary to Medicare?
Do you have employer group health plan (GHP) coverage through yourself, a spouse, or family member if dually entitled based on Disability and ESRD? If yes, the employer GHP may be primary to Medicare. Continue below.
Does Medicare require independent labs to collect MSP?
The Centers for Medicare & Medicaid Services (CMS) will not require independent reference laboratories to collect MSP information in order to bill Medicare for reference laboratory services as described in subsection (b) above. Therefore, pursuant to section 943 of The Medicare Prescription Drug, Improvement & Modernization Act of 2003, CMS will not require hospitals to collect MSP information in order to bill Medicare for reference laboratory services as described in subsection (b) above. This policy, however, will not be a valid defense to Medicare’s right to recover when a mistaken payment situation is later found to exist.
Can you send a claim to Medicare with multiple primary payers?
Claims with multiple primary payers cannot be sent electronically to Medicare.
What is MSP in Medicare?
MSP provisions prevent Medicare paying items and services when patients have other primary health insurance coverage. In these cases, the MSP Program contributes:
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is a term used when Medicare is not responsible for paying first on a healthcare claim. The decision as to who is responsible for paying first on a claim and who pays second is known in the insurance industry as “coordination of benefits.”
What is Medicare data match?
This data match identifies persons that have had earnings in a given tax year. If a Medicare beneficiary and/or the spouse of a beneficiary has had earnings, that signifies employment, which means it is possible they also had Group Health Plan insurance coverage. A questionnaire is then sent to the employer inquiring about possible coverage that is primary to Medicare. If coverage exists or existed, dates of coverage are obtained, as well as the name and address of the insurer. Records obtained through this process are generally very reliable. 21
What is a group health plan?
A Group Health Plan is health coverage sponsored by an employer or employee organization (such as a union) for a group of employees, and possibly for dependents and retirees as well. The term GHP includes self-insured plans, plans of government entities (Federal, State, and local), and employee organization plans such as union plans, employee health and welfare funds, or other employee organization plans. The term also includes “employee-pay-all” plans which receive no financial contributions from the employer. The term does not include self-employed persons. 7
Is Medicare a non group health plan?
Non-Group Health Plan MSP encompasses three different types of insurance: Liability, No- Fault, and Workers’ ompensation. y statute, Medicare is always a secondary payer to Liability insurance (including Self-insurance). An example of Liability insurance is where a Medicare beneficiary is injured in an auto accident. The beneficiary files a claim against the alleged responsible party and receives payment. Medicare is the secondary payer to the Liability insurance payment.
Is Medicare a primary or secondary payer?
We just addressed the fact that Medicare is always the secondary payer of benefits to Non-Group Health Plan insurance, and when certain conditions are met, the secondary payer to Group Health Plan insurance. If Medicare is not aware of other primary insurance, Medicare may mistakenly pay as primary.
Is Medicare Supplement the same as Medicare Secondary Payer?
The term Medicare supplement (i. e., Medigap) should not be confused with Medicare Secondary Payer. Medicare supplemental is a private health insurance policy designed specifically to fill some of the “gaps” in Medicare’s coverage when Medicare is the primary payer. Medigap policies typically pay for expenses that Medicare does not pay for, such as deductible or coinsurance amounts or other limits under the Medicare program. Private "Medigap" insurance and Medicare secondary payer law and regulations are not the same. A “Medigap” policy is not a Medicare program benefit.