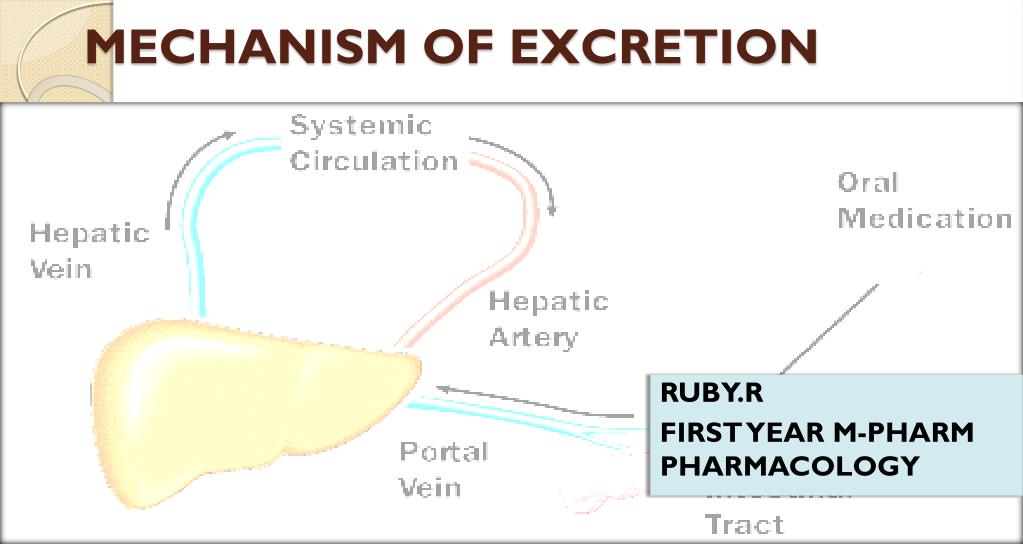
What is meant by excretion of drugs?
Excretion is the passage out of systemically absorbed drug. Drugs and their metabolites are excreted in: Excretion is the passage out of systemically absorbed drug. Drugs and their metabolites are excreted in: Through the kidney. It is the most important channel of excretion for majority of drugs (see below).
What is excreted from the body?
Excretion is the removal of drugs and their metabolites from the body. The kidney is the principal drug-excreting organ. The three components of renal excretion, i.e. glomerular filtration, secretion, and reabsorption, are introduced in a brief video from Handwritten Tutorials (see the Learning Resources at the end of this topic).
How do intrinsic properties of a drug affect excretion?
In addition, excretion of a drug is dependent on intrinsic properties of the drug, such as pH and size. For example, weakly acidic drugs display increased excretion in basic urine, while weakly basic drugs are excreted more readily in acidic urine.
What is the mechanism of excretion of drugs from saliva?
Saliva often contains very small quantities of drug and this may be regarded as a mechanism of excretion although the amount is inconsequential in companion animal species. The gastrointestinal tract can also be involved in elimination of some drugs.

What is the difference between excretion and elimination in pharmacology?
Elimination is the removal of a medication from the body. Now this can be accomplished through metabolism, where the medication is broken down into inactive metabolites, or through excretion which is when the intact medication is transported out of the body.
What is meant by drug metabolism and excretion?
Metabolites may be metabolized further instead of being excreted from the body. The subsequent metabolites are then excreted. Excretion involves elimination of the drug. (See also Introduction to Administration and Kinetics of Drugs.) All drugs are eventually eliminated from the body.
What is absorption and excretion?
Absorption is the transfer of a chemical from the site of exposure, usually an external or internal body surface, into the systemic circulation. Toxicants are removed from the systemic circulation by biotransformation, excretion, and storage at various sites in the body.
What are the four routes of excretion?
The most important routes for excretion are urine, feces, and exhaled air. Other minor routes of excretion include milk, sweat, saliva, tears, hair, and nails.
Where does drug excretion occur?
Drug excretion primarily occurs through the kidney and liver (seeFig. 45.2). The kidney uses three mechanisms of drug excretion: glomerular filtration, active secretion through the proximal tubules, or distal tubule reabsorption.
Which organ is mostly involved in drug excretion?
Although many sites of metabolism and excretion exist, the chief organ of metabolism is the liver, while the organ primarily tasked with excretion is the kidney. Any significant dysfunction in either organ can result in the accumulation of the drug or its metabolites in toxic concentrations.
What are the differences between excretion and secretion?
But the difference between excretion and secretion is that excretion is the removal of waste from the body, whereas secretion involves the movement of materials within the body.
Is sweat a secretion or excretion?
For an example of excretion, humans excrete such materials as tears, feces, urine, carbon dioxide, and sweat while secretion, on the other hand, includes enzymes, hormones, or saliva.
What are the 3 phases of drug action?
A tablet or capsule taken by mouth goes through three phases—pharmaceutic, pharmacokinetic, and pharmacodynamic—as drug actions occur. In the pharmaceutic phase, the drug becomes a solution so that it can cross the biologic membrane.
What are the types of excretion?
Modes of ExcretionAmmonotelism (Type of excretion- ammonia)Ureotelism (Type of excretion – urea)Uricotelism (Type of excretion – uric acid)Aminotelism (Type of excretion – amino acids)Guanotelism (Type of excretion – guanine)
What is excretion example?
Excretion is an essential process in all forms of life. For example, in mammals, urine is expelled through the urethra, which is part of the excretory system. In unicellular organisms, waste products are discharged directly through the surface of the cell.
Why is excretion important?
Excretion is the removal of waste materials arising from normal life processes from the body. It is necessary to eliminate waste products, such as carbon dioxide. They cause poisoning that slows down critical chemical reactions if they are left to accumulate.
What metabolism means?
Metabolism is the process by which your body converts what you eat and drink into energy. During this complex process, calories in food and beverages are combined with oxygen to release the energy your body needs to function.
What is the purpose of drug metabolism?
Drug metabolism is the term used to describe the biotransformation of pharmaceutical substances in the body so that they can be eliminated more easily. The majority of metabolic processes that involve drugs occur in the liver, as the enzymes that facilitate the reactions are concentrated there.
What are the 3 phases of metabolism?
The metabolism of xenobiotics is often divided into three phases:- modification, conjugation, and excretion. These reactions act in concert to detoxify xenobiotics and remove them from cells.
What are the 2 phases of drug metabolism?
Phase I reactions of drug metabolism involve oxidation, reduction, or hydrolysis of the parent drug, resulting in its conversion to a more polar molecule. Phase II reactions involve conjugation by coupling the drug or its metabolites to another molecule, such as glucuronidation, acylation, sulfate, or glicine.
What is the removal of drugs and their metabolites from the body?
Excretion is the removal of drugs and their metabolites from the body.
What excretion is smaller than urine?
Other excretion. Excretion with the bile (and thereby with feces), sweat, exhaled air, saliva, and breast milk play a much smaller role compared to urine. An exception is the excretion of volatile anesthetics with ex haled air.
Why does renal excretion decrease with age?
In most people renal drug excretion decreases with age, chiefly due to the physiological decline of the glomerular filtration, but also as a result of various kidney diseases.
How long is the renal excretion video?
This is a seven minute animated video introducing the processes involved in renal excretion.
Why is excretion important in breast milk?
The particular importance of the excretion via breast milk lies in the toxic effects of some drugs on the breastfeeding infant. Note that substance-specific portions of orally administered drugs are removed with feces without entering the circulation.
What is the least affected by hepatic drug metabolism?
Least affected are hydrophilic, i.e. polar or ionized drugs, due to their inability to cross the membranes of nephron cells. Reducing reabsorption via increasing hydrophilicity is the primary task of hepatic drug metabolism.
What is the passage out of systemically absorbed drugs?
Excretion is the passage out of systemically absorbed drug. Drugs and their metabolites are excreted in:
Which drugs are reabsorbed by bacteria in the intestines?
Most of the drug, including that released by deconjugation of glucuronides by bacteria in intestines is reabsorbed (enterohepatic cycling) and ultimate excretion occurs in urine. Drugs that attain high concentrations in bile are erythromycin, ampicillin, rifampin, tetracycline, oral contraceptives, phenolphthalein.
What are the substances that are present in saliva?
These are of minor importance for drug excretion. Lithium, pot. iodide, rifampin and heavy metals are present in these secretions in significant amounts. Most of the saliva along with the drug in it, is swallowed and meets the same fate as orally taken drug.
How do drugs enter breast milk?
Most drugs enter breast milk by passive diffusion. As such, more lipid soluble and less protein bound drugs cross better.
What causes drug excretion?
Genetic variation and underlying acute or chronic comorbidities can also impact drug excretion. Impaired kidney function or hepatic diseases that compromise biotransformation pathways may decrease drug excretion, which can result in drug accumulation and potential toxicity.
How are excreted drugs eliminated?
Excreted drugs are either eliminated in their original, unmetabolized form, or they can be eliminated following metabolic biotransformation, as described in the preceding chapters. The metabolic biotransformation prepares drugs for excretion.
How to calculate total drug excretion?
Total medication clearance is described by CL = CL k + CL h + CL other where CL k reflects kidney clearance, CL h reflects hepatic clearance, and CL other integrates all other sources such as extracorporeal clearance as with renal replacement therapy or metabolism by pH-dependent plasma esterases ( Lea-Henry et al., 2018 ). As can be seen in the preceding equation, the main contributors to drug excretion are the kidneys and the liver. Water-soluble compounds are excreted primarily by the kidneys, while larger, more hydrophobic compounds are the responsibility of the liver. Secondary routes of excretion do exist (CL other ), such as through breast milk, sweat, saliva, hair, and respiration. However, their contribution tends to be small. The following chapter will describe the various routes of excretion, the methods by which researchers and clinicians measure and model drug excretion, and how this information may be applied clinically.
What is the process of converting phenytoin to water soluble metabolites?
A series of metabolic transformations in the liver convert phenytoin to several inactive water-soluble metabolites that can then be excreted in the urine. In addition, excretion of a drug is dependent on intrinsic properties of the drug, such as pH and size.
Where does the most drug excretion occur?
The greatest proportion of drug excretion occurs through the kidneys . The liver makes most drugs and remedies water soluble for removal via the kidneys (see Figure 17.1, p. 131 ). One-fifth of the plasma reaching the kidney glomerulus is filtered through the pores in the glomerular cell membrane.
Which organs are responsible for excretion of drugs?
By far, the most important excretory organs are the kidney and liver. In kidney, excretion of drugs depends on glomerular filtration, active tubular secretion, and passive tubular absorption.
Which organ excretes water soluble compounds?
Water-soluble compounds are excreted primarily by the kidneys, while larger, more hydrophobic compounds are the responsibility of the liver. Secondary routes of excretion do exist (CL other ), such as through breast milk, sweat, saliva, hair, and respiration. However, their contribution tends to be small.
What system is responsible for excretion of drugs?
The biliary system contributes to excretion to the degree that drug is not reabsorbed from the gastrointestinal (GI) tract. Generally, the contribution of intestine, saliva, sweat, breast milk, and lungs to excretion is small, except for exhalation of volatile anesthetics. Excretion via breast milk may affect the breastfeeding infant (see table ...
Which organs excrete drugs?
Drug Excretion. The kidneys are the principal organs for excreting water-soluble substances. The biliary system contributes to excretion to the degree that drug is not reabsorbed from the gastrointestinal (GI) tract. Generally, the contribution of intestine, saliva, sweat, breast milk, and lungs to excretion is small, ...
Why are drugs excreted in the bile?
Some drugs and their metabolites are extensively excreted in bile. Because they are transported across the biliary epithelium against a concentration gradient, active secretory transport is required. When plasma drug concentrations are high, secretory transport may approach an upper limit (transport maximum). Substances with similar physicochemical properties may compete for excretion.
What are the principles of transmembrane passage?
The principles of transmembrane passage govern renal handling of drugs. Drugs bound to plasma proteins remain in the circulation; only unbound drug is contained in the glomerular filtrate. Un-ionized forms of drugs and their metabolites tend to be reabsorbed readily from tubular fluids.
How are cations and anion transports handled?
Anions and cations are handled by separate transport mechanisms. Normally, the anion secretory system eliminates metabolites conjugated with glycine, sulfate, or glucuronic acid. Anions compete with each other for secretion. This competition can be used therapeutically; eg, probenecid blocks the normally rapid tubular secretion of penicillin, resulting in higher plasma penicillin concentrations for a longer time. In the cation transport system, cations or organic bases (eg, pramipexole, dofetilide) are secreted by the renal tubules; this process can be inhibited by cimetidine, trimethoprim, prochlorperazine, megestrol, or ketoconazole.
What is the effect of alkalinization on urine?
In some cases of overdose, these principles are used to enhance the excretion of weak bases or acids; eg, urine is alkalinized to enhance excretion of acetylsalicylic acid.
Which drugs inhibit the cation transport system?
In the cation transport system, cations or organic bases (eg, pramipexole, dofetilide) are secreted by the renal tubules; this process can be inhibited by cimetidine, trimethoprim, prochlorperazine, megestrol, or ketoconazole.
What is excreted from the kidney?
Milk. Faeces. Bile. Drugs are excreted from the kidney by glomerular filtration and by active tubular secretion following the same steps and mechanisms as the products of intermediate metabolism. Therefore, drugs that are filtered by the glomerulus are also subject to the process of passive tubular reabsorption.
What is the definition of elimination in pharmacology?
In pharmacology the elimination or excretion of a drug is understood to be any one of a number of processes by which a drug is eliminated (that is, cleared and excreted) from an organism either in an unaltered form (unbound molecules) or modified as a metabolite.
What is the definition of pharmacokinetics?
Pharmacokinetic parameters of elimination. Pharmacokinetics studies the manner and speed with which drugs and their metabolites are eliminated by the various excretory organs. This elimination will be proportional to the drug's plasmatic concentrations. In order to model these processes a working definition is required for some ...
What does globular filtration remove?
Glomerular filtration will only remove those drugs or metabolites that are not bound to proteins present in blood plasma (free fraction) and many other types of drugs (such as the organic acids) are actively secreted.
What is the half life of a drug?
Half life. The plasma half-life or half life of elimination is the time required to eliminate 50% of the absorbed dose of a drug from an organism. Or put another way, the time that it takes for the plasma concentration to fall by half from its maximum levels.
Why is it important to know if a drug is likely to be eliminated from a woman's body?
The liver and kidneys of newly born infants are relatively undeveloped and they are highly sensitive to a drug's toxic effects. For this reason it is important to know if a drug is likely to be eliminated from a woman's body if she is breast feeding in order to avoid this situation.
When is the steady state of a drug reached?
The steady state or stable concentration is reached when the drug's supply to the blood plasma is the same as the rate of elimination from the plasma. It is necessary to calculate this concentration in order to decide the period between doses and the amount of drug supplied with each dose in prolonged treatments.
What is the absorption of a drug?
In pharmacokinetics, absorption is how a medication gets from the site of administration into the bloodstream.
What is distribution in pharmacokinetics?
In pharmacokinetics, distribution is how a medication gets from the bloodstream to the site of action.
What is pharmacokinetics?
Pharmacokinetics is the study of movement and processing of drugs within the body.
How does the absorption rate of a medication change as you get older?
Other things could include the surface area of the absorption site as well as the presence of food in the stomach and the pH of the stomach acid. So as we get older, our pH increases, becomes more alkaline, and that really decreases absorption of a medication. So as we get older, absorption rate decreases.
How does IV medication affect absorption?
The delivery route of a medication affects absorption. A medication administered via IV goes straight into the bloodstream, so absorption is immediate. However, an oral medication has to go through the GI tract, so absorption is a little slower.
How does solubility affect absorption?
The solubility, dose, and formulation of the medication affect absorption. For example, a liquid medication will be absorbed quicker than a tablet.
Why is the kidney responsible for toxicity?
Because the kidneys and liver are primarily responsible for excretion, kidney or liver dysfunction can result in less excretion, and therefore, potential drug buildup and toxicity.
Where are drug metabolizing enzymes expressed?
They are therefore expressed also at other interfaces of the body with the environment such as the skin, lungs, and the kidney.
What are the organs of drug metabolism?
The principal organs of drug metabolism are the liver and (for orally taken drugs) the small intestine. Drugs completely inactivated during the first-pass through these organs must be given parenterally, similarly to poorly absorbed drugs.
What is the primary objective of drug metabolism?
Drug metabolism. The primary objective of drug metabolism is to facilitate a drug’s excretion by increasing its water solubility (hydrophilicity). The involved chemical modifications incidentally decrease or increase a drug’s pharmacological activity and/or half-life, the most extreme example being the metabolic activation ...
Is hepato-intestinal drug metabolism variable?
Hepato-intestinal drug metabolism is highly variable not only among patients but even in one particular individual over time. It is lower immediately after birth, in carriers of inactivating mutations in drug metabolizing enzymes, in patients treated with drugs inhibiting these enzymes ( e.g. macrolids and conazols), and in those with liver disease or insufficient hepatic blood flow. It is higher in patients treated with transcriptional inducers of drug metabolizing enzymes, e.g. with rifampin or carbamazepine and, in the case of CYP2D6, in the presence of additional gene copies. The induction and inhibition of drug metabolism constitute examples of pharmacokinetic drug interactions. As drug metabolizing enzymes also metabolize certain endobiotics, induction and inhibition may result in metabolic disorders.
Is CYP2D6 higher in patients treated with transcriptional inducers of drug metabolizing enzyme?
It is higher in patients treated with transcriptional inducers of drug metabolizing enzymes, e.g. with rifampin or carbamazepine and, in the case of CYP2D6, in the presence of additional gene copies.