What is the normal range of right ventricular function?
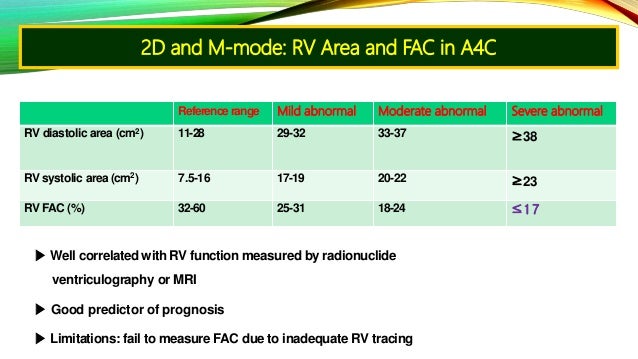
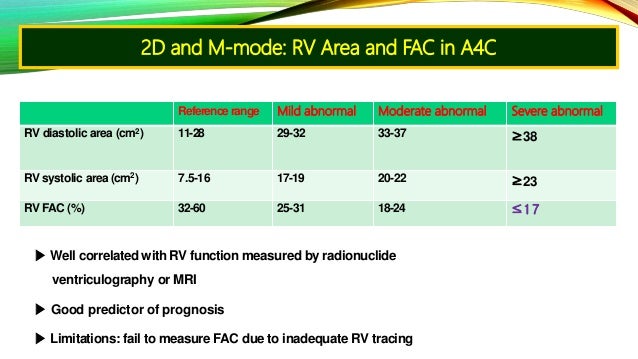
Right ventricular function Reference range Mildly abnormal Moderately abnormal Severely abnormal * RV fractional area change, % 32–60 25–31 18–24 ≤17 * TAPSE, cm 1.5-2.0 1.3-1.5 1.0-1.2 <1.0 * RV MPI <0.28 * Dp/DT >400mmHg 2 more rows ...
When is the right ventricle considered to be enlarged?
On contrast-enhanced chest CT and cardiac MRI, the right ventricle when measured on axial slices can be considered enlarged when the transverse diameter is ≥60 mm (male) and ≥57 mm (female) 4. On transthoracic echocardiography the right ventricle can be considered enlarged when 5: the basal diameter exceeds 42 mm.
How thick is the muscular wall of the right ventricle?
MUSCULATURE OF VENTRICULAR WALL. In the normal heart, the muscular wall of the right ventricle not including trabeculations is 3–5 mm thick. 7 In this relatively thin wall circumferential and longitudinal orientations predominate. In contrast, the thicker left ventricular wall contains obliquely arranged myofibres,...
What is the anatomy of the right ventricle?
Gross anatomy. The right ventricle projects to the left of the right atrium and when viewed in the cardiac short axis plane, is semilunar in shape wrapping around the anterolateral aspect of the left ventricle. It has thinner walls than the left ventricle due to lower right sided pressures compared to the left ventricle.

What is mild enlarged right ventricle?
Right ventricular hypertrophy (also called right ventricular enlargement) happens when the muscle on the right side of your heart becomes thickened and enlarged. When your heart gets larger, it's more prone to wear out.
What is normal right ventricular wall thickness?
In the normal heart, the muscular wall of the right ventricle not including trabeculations is 3–5 mm thick. In this relatively thin wall circumferential and longitudinal orientations predominate.
How thick is the right ventricle in CM?
The mean (1 SD) thickness of the right ventricular free wall measured at a total of 512 points was 0.44 (0.12) cm in patients with hypertrophic cardiomyopathy, 0.29 (0.08) cm in healthy individuals, and 0.73 (0.27) cm in patients with pulmonary hypertension.
What is the normal size of a left ventricle?
These criteria classify the LV size as normal (men: 42 to 59 mm; women: 39 to 53 mm), mildly dilated (men: 60 to 63 mm; women: 54 to 57 mm), moderately dilated (men: 64 to 68 mm; women: 58 to 61 mm), or severely dilated (men: ≥69 mm; women: ≥62 mm).
Why is my right ventricle enlarged?
Right ventricular hypertrophy is a thickening of the heart's lower right chamber due to pressure overload. This makes it harder for the heart to pump blood to the lungs. The most common causes of right ventricular hypertrophy are severe lung disease, a leaky tricuspid heart valve, or certain genetic heart conditions.
What causes enlarged right side of heart?
High blood pressure in the arteries in the lungs (pulmonary hypertension). The heart has to work harder to move blood between the lungs and the heart. The strain may lead to thickening or enlargement of the right side of the heart.
How do you measure right ventricle?
0:284:24Measuring the right ventricle in echocardiography - YouTubeYouTubeStart of suggested clipEnd of suggested clipPoint between the aortic valve and the interventricular septum and measuring vertically up towardMorePoint between the aortic valve and the interventricular septum and measuring vertically up toward the right ventricular endocardium.
Are the left and right ventricles different sizes?
In parasagittal and coronal scans through the posterior horn of the lateral ventricle, the lateral ventricle was traced and its area was measured. We found no significant variation of ventricular size in relation to body weight at birth. The left ventricular size was larger than the right one.
What is the size of the ventricle?
DimensionsDimensionAbbreviationNormallyLeft ventricular end diastolic posterior wall dimensionLVPWd8.3 mm, Range 7 – 11 mmMean left ventricular myocardial thicknessMean LVMTWomen: 4 - 8 mm Men: 5 - 9 mmMean right ventricular myocardial thicknessMean RVMT4 - 7 mmLeft ventricular end systolic dimension16 mm8 more rows
What percentage of heart function can you live with?
A normal heart pumps blood out of its left ventricle at about 50 to 70 percent — a measurement called an ejection fraction, according to the American Heart Association. “Don was at 10 percent, which is basically a nonfunctional heart,” Dow said. “When a heart is pumping at only 10 percent, a person can die very easily.
What is a normal ejection fraction by age?
An ejection fraction range between 41 and 51 percent for men and between 41 and 53 percent for women is classified as mildly reduced....What do ejection fraction results mean?LVEF rangeMenWomenNormal range52–72%54–74%Mildly abnormal range41–51%41–53%Moderately abnormal range30–40%30–40%1 more row
What is a good ejection fraction?
A normal ejection fraction is about 50% to 75%, according to the American Heart Association. A borderline ejection fraction can range between 41% and 50%.
What is LV wall thickness?
This study found that the LV was thickest in the basal septum (segment 3) with a mean thickness of 8.3 mm and 7.2 mm and thinnest in the midventricular anterior wall (segment 7) with 5.6 mm and 4.5 mm for men and women, respectively (16).
How common is right ventricular hypertrophy?
RVH is seen in 76% of patients with advanced COPD and 50% of patients with restrictive lung disease. RVH also occurs in response to structural defects in the heart. One common cause is tricuspid insufficiency.
What is the significance of the difference in thickness of the right and left ventricular walls?
The left ventricle of your heart is larger and thicker than the right ventricle. This is because it has to pump the blood further around the body, and against higher pressure, compared with the right ventricle.
What would you most likely see in right ventricular hypertrophy?
Right ventricular hypertrophy causes large R-waves in right-sided chest leads and deeper S-waves in left-sided leads.
What is the right ventricle?
The right ventricle in the normal heart is the most anteriorly situated cardiac chamber since it is located immediately behind the sternum. It also marks the inferior border of the cardiac silhouette. In contrast to the near conical shape of the left ventricle, the right ventricle is more triangular in shape when viewed from the front and it curves over the left ventricle. When seen from the apex, the right edge of the right ventricle is sharp, forming the acute margin of the heart. In cross section the cavity appears like a crescent. Thus, the curvature of the ventricular septum places the right ventricular outflow tract antero‐cephalad to that of the left ventricle's resulting in a characteristic “cross over” relationship between right and left ventricular outflows (fig 11). This important spatial relationship is one of the fundamental prerequisites for sonographers screening for congenital heart malformations since clinically important heart malformations such as complete transposition may be present when the outlets lack the “cross over” sign.
What are the three parts of the right ventricle?
The cavity of the chamber can be described in terms of three component parts: inlet, apical trabecular, and outlet as suggested by Goor and Lillehei (fig 2B2B).2In the analysis of congenitally malformed hearts, this tripartite concept is more useful than the traditional division of the right ventricle into sinus and conus components. In malformed hearts, one or more of the three components may be lacking in one ventricle. The affected ventricle is usually smaller than its counterpart on the other side but is also incomplete and described as rudimentary. Very rarely, the heart contains only one ventricular chamber—the truly univentricular heart with a solitary ventricle.
What is the myocardium?
The myocardium is a complex three dimensional network of myocytes in a matrix of fibrous tissue. Each myocyte is long and thin and joined to its neighbour at the ends as well as at its side branches. There is then a predominant longitudinal orientation of the myocytes forming the myofibres. The architecture or gross arrangement of these myofibres have been studied over more than 300 years with somewhat different interpretations among investigators primarily owing to technical difficulties in “tracing” each myofibre network in three dimensions without disturbing adjoining fibres.6Since these contractile bundles change the shape of the heart and generate the force of the pumping chambers during systole, a summary of the arrangement of myofibres in the right ventricle can help the echocardiographer in understanding its function. The superficial or subepicardial myofibres are arranged more or less circumferentially in a direction that is parallel to the atrioventricular groove and encircle the subpulmonary infundibulum (fig 33). On the sternocostal aspect, the superficial fibres turn obliquely toward the cardiac apex to cross the interventricular groove and continue into the superficial myofibres of the left ventricle. On the diaphragmatic aspect, superficial right ventricular fibres turn a slight angle toward the base to join left ventricular myofibres. At the right ventricular apex, superficial myofibres invaginate in spiral fashion to form the deep or subendocardial myofibres that line the cavity. The deep myofibres are longitudinally aligned, apex to base (fig 33). In the normal heart, the muscular wall of the right ventricle not including trabeculations is 3–5 mm thick.7In this relatively thin wall circumferential and longitudinal orientations predominate. In contrast, the thicker left ventricular wall contains obliquely arranged myofibres, superficially and longitudinal myofibres in the subendocardium, but these sandwich predominantly circular myofibres in between. Interestingly, our study on the hypertrophied right ventricle in tetralogy of Fallot showed a change in architecture to resemble the sandwich pattern seen in the normal left ventricle.8
What is the ventricular septum?
The ventricular septum is muscular apart from a very small fibrous portion that is the membranous septum. Ventricular septal defects that occur in the environs of the membranous septum are described as perimembranous defects. Owing to the curvature of the ventricular septum in the normal heart (fig 2A2A),), the right ventricle is described as wrapping around the left ventricle. However, the configuration of the left ventricular inlet and outlet portions does not allow the corresponding portions of the right ventricle to be superimposed upon each other. The overlap between left ventricular inlets and outlets puts the aortic outflow tract immediately behind the septum that separates it from the right ventricular inlet, reflecting the “wedged” position of the aortic root (fig 2A2A).
What is crux of heart?
The term “crux” of the heart (crus cordis) refers to the intersection between the planes of the atrial and ventricular septa upon the inferior atrioventricular junction. However, close examination will show the crux is not a perfect cross since the right atrioventricular junction is inferior to that of the left.1Nevertheless, this view shows how the four chamber echocardiographic plane can be achieved. The most inferior sections will traverse the coronary sinus running alongside the inferior wall of the left atrium (fig 11).
Why is it necessary to image the right ventricle from several projections?
Because of the complex shape of the right ventricle, triangular from the frontal aspect and crescentic from the apex , it is necessary to image the right ventricle from several projections, each characterised by specific anatomic landmarks.
Where is the pulmonary valve located?
The pulmonary valve is separated from the tricuspid valve by a muscular fold, the ventriculo‐infundibular fold. The fold forms the supraventricular crest at its septal margin where it inserts between the anterior and posterior limbs of the septomarginal trabeculation (fig 2B,D2B,D). From its septal margin, the fold continues superiorly into the subpulmonary infundibulum of the right ventricular outlet. The antero‐superior wall of the right ventricle completes the muscular tube known as the subpulmonary infundibulum that leads to the pulmonary valve (fig 2D2D). Significantly, it is possible surgically to detach the infundibulum so as to harvest the entirety of the pulmonary valve for use as an autograft in the Ross procedure without incursion into the left ventricle.5Thus, the infundibulum lifts the pulmonary valve clear of the ventricular septum. The semilunar hingelines of the pulmonary valve cross the anatomic junction between ventricular muscle and the fibro‐elastic wall of the pulmonary trunk (fig 2D2D). In this arrangement, small segments of infundibular muscle are enclosed within the three pulmonary sinuses. The apices of the hingelines attach to the sinutubular junction that demarcates the juncture between the sinuses and the tubular portion.
What is the formula for right ventricular volumetry?
Right ventricular volumetry was accomplished using “ellipsoidal shell model” with corresponding formula V =2/3 Pd . Area P was measured in our modification of apical four-chamber view and distance d in parasternal short axis. All measurements were performed in both systole and diastole. The difference of enddiastolic (EDV) and endsystolic volume (ESV) yielded stroke volume (SV). SV expressed as percentage of EDV represents RV EF. Exact specification of projections and validation of the model and method used was carried out on a group of 82 patients as published before. 7
What is the normal RV EF?
Normal mean value of RV EF is 53.9%. The lower range in males is 40% and in females 45%.
Is MRI considered RV volumetry?
At present several methods enable non-invasive quantification of RV volumes and EF (MRI, 1–3 radionuclides 4,5 and echocardiography 6,7 ). There is a little experience in RV volumetry generally. Though MRI is considered the gold standard in RV volumetry, 1–3 the selection of preferred method is influenced also by its availability, cost, patient's comfort and repeatability during follow-up, therefore echocardiography might be preferred. Our experience as well as recent literature indicate that echocardiography is a relatively easy and reliable also in this respect. 6,7
Is EDVI lower in males than females?
When comparing male and female patients, EDVI and ESVI of the RV in males exceed significantly those in females, which in turn explains the significantly lower RV EF in males as compare to females ( Fig. 5 ). In contrast LV EF in both males and females did not show any significant difference ( Table 2 ). RV and LV EF of the persons in our study were not dependent on the age ( Fig. 6 ).
Is EDV greater than LV?
The indexed EDV (EDVI) and ESV (ESVI) of the RV were significantly greater than those of the LV (pair t -test, α =0.1%). There was no significant difference between indexed SV (SVI) of the RV and LV. This supports the validity of the RV volumetric method used. EF of the RV is significantly lower than that of the LV (pair t -test, α =0.1%).
What is the normal thickness of myocardial wall?
Parasagittal “white blood ” MRI sequence throuGh the normal reveal myocardial thickness in the 5mm range of the inferior and anterior wall
What is the lateral X-ray of the left ventricle?
A normal lateral examination of the chest X-ray is shown to exemplify the positioning of the cardiac chambers showing the right ventricular outflow tract (RVOT) anteriorly, the left atrium (LA) posteriorly and superiorly, the left ventricle (LV) posteriorly and inferiorly and the inferior vena cava (IVC) as a separate shadow posterior to the LV.
What portion of the diaphragmatic surface does the heart take up?
In the P-A projection the normal heart takes up about 30% of the diaphragmatic surface. Similarly in the lateral projection the heart takes up a third of the diaphragmatic surface. In addition the heart takes up the bottom 1/3 of the retrosternal air space.
What heart shape did CXR show?
CXR showed cardiomegaly with a triangular shaped heart
Which part of the heart is difficult to measure?
The Right Ventricle. The contractile function of the RV is difficult to measure due to its complex anatomy. Historically, there has been very little attention paid to this part of the heart since it was assumed that the RV only played a passive role.
What is the time interval for differential pressure of 12 mmHg?
Therefore, by definition, the time interval for a differential pressure of 12mmHg is assessed (4V^2) . This number, 12, is divided by the time interval in seconds, a result less than 400 mmHg/sec is an indication for a reduced right ventricular function.
What is the pressure gradient between the right ventricle and the atrium?
In the example in fig 3, the maximum tricuspid regurgitation signal is 2.3 m/s; therefore, the pressure gradient between the right ventricle and the atrium is 21 mm Hg. The final calculation depends on an estimated value of the right atrial pressure that is conventionally based on both the size of the inferior vena cava and the change in calibre of this vessel with respiration. In a normal patient, 5–10 mm Hg is usually considered normal. Therefore, in this example the final pulmonary artery systolic pressure is 31 mm Hg.
How are echocardiographic variables calculated?
All echocardiographic variables were calculated using the commercially available software EchoPAC PC V6.00 (GE Vingmed Ultrasound) and determined by a single observer. Three measurements were collected for each variable, and the mean (SD) of each variable was used for comparison analysis using the two-tailed Student t test for paired and unpaired data. Linear regression analysis was used to examine relations between various dependent variables. Univariate analysis between PASP and other echocardiographic variables was also performed. The ability of the measured echocardiographic variables of RV size and systolic function to detect an abnormal PASP greater than 40 mm Hg, considered as abnormal, was assessed using receiver-operating characteristic curves to provide optimal values for each variable and areas under the curve (AUCs), which were compared by the method of Hanley and McNeil. 19 Finally, a stepwise multiple linear regression analysis was performed to determine the independent predictive value of the echocardiographic variables with respect to PH. p<0.05 was considered significant.
What is the name of the blood vessel that leads from the heart to the lungs?
Pulmonary hypertension is a rare blood vessel disorder of the lung in which the pressure in the pulmonary artery (the blood vessel that leads from the heart to the lungs) rises above normal levels and may become life threatening.
Can RV size be used in routine evaluation?
In summary, these results provide a range of normal variables of RV size and function, not previously published, that can be used in the routine evaluation and follow-up of patients with PH, with the implication that, by knowing and applying these variables, we will be able to determine RV dysfunction earlier and therefore diagnose PH earlier.
What is the transverse diameter of the right ventricle?
On contrast-enhanced chest CT and cardiac MRI, the right ventricle when measured on axial slices can be considered enlarged when the transverse diameter is ≥60 mm (male) and ≥57 mm (female) 4.
What is the shape of the ventricular septum?
It is separated from the left ventricle by the interventricular (IV) septum, which is concave in shape (i.e. bulges into the right ventricle). It has three walls named anterior, inferior, and septal. The interior ventricular surface has irregular muscular ridges known as trabeculae carneae.
What is the determinant of right ventricle contraction?
Contraction of the right ventricle occurs in sequence, initiated by the inlet and apical regions followed by outflow/infundibular contraction. In contrast to the left ventricle, longitudinal shortening is the primary contractile determinant of right ventricular stroke volume; this facet of right ventricular function is appreciated clinically by the excursion of the tricuspid annulus, drawn toward the apex with each systole. An inward "bellows-like" motion of the right ventricular free wall and traction from left ventricular contraction also contribute to overall systolic function 7 .
What is the name of the ridges on the ventricular surface?
The interior ventricular surface has irregular muscular ridges known as trabeculae carneae. A prominent trabecula, the supraventricular crest, separates the trabeculated inferior ventricle from the smooth wall of the right ventricular outflow tract. It acts to redirect blood approximately 140° from the inflow tract to the outflow tract.
What is the primary contractile determinant of right ventricular stroke volume?
Contraction of the right ventricle occurs in sequence, initiated by the inlet and apical regions followed by outflow/infundibular contraction. In contrast to the left ventricle, longitudinal shortening is the primary contractile determinant of right ventricular stroke volume; this facet of right ventricular function is appreciated clinically by the excursion of the tricuspid annulus, drawn toward the apex with each systole. An inward "bellows-like" motion of the right ventricular free wall and traction from left ventricular contraction also contribute to overall systolic function 7 .
What is the inflow part of the ventricle?
The inflow part of the ventricle receives blood from the right atrium via the tricuspid valve. The fibrous ring surrounding the valve forms part of the fibrous skeleton of the heart. Superiorly the chamber tapers as the funnel-shaped outflow tract, known as the conus arteriosus (or infundibulum ), which lack trabeculae and continues beyond the pulmonary valve as the pulmonary trunk.
What is the RV in the heart?
The right ventricle ( RV) is the most anterior of the four heart chambers. It receives deoxygenated blood from the r ight atrium (RA) and pumps it into the pulmonary circulation. During diastole, blood enters the right ventricle through the atrioventricular orifice through an open tricuspid valve (TV). During systole, blood is ejected ...
How to know if you have right ventricular hypertrophy?
However, if you have right ventricular hypertrophy due to an underlying lung condition, such as pulmonary arterial hypertension, you might notice symptoms, including. chest pain/pressure. dizziness. fainting. shortness of breath. swelling in the lower extremities, such as the ankles, feet, and legs.
What side of heart looks bigger on chest xray?
Chest X-ray. This allows your doctor to see whether the right side of your heart looks larger than usual.
What is the difference between the left and right side of the heart?
Your heart is divided into a left and a right side. The right side of your heart pumps blood to your lungs to receive oxygen. The left side pumps the oxygenated blood to the rest of your body. Right ventricular hypertrophy (also called right ventricular enlargement) happens when the muscle on the right side of your heart becomes thickened ...
What is the best medicine for right ventricular hypertrophy?
digoxin (Lanoxin) diuretics. If right ventricular hypertrophy is making it hard for your heart to beat consistently, you may also need a pacemaker. This is a device that helps your heart maintain a regular rhythm.
Can right ventricular hypertrophy cause symptoms?
Right ventricular hypertrophy doesn’t always cause symptoms. Often, the left ventricle tries to compensate for the problems with the right ventricle. This means that some people don’t know they have right ventricular hypertrophy until it’s more advanced.
Can left ventricular hypertrophy cause congestive heart failure?
If left untreated, right ventricular hypertrophy can increase your risk of congestive heart failure. If you do have right ventricular hypertrophy, make sure to closely follow the treatment plan recommended by your doctor.