What is the periapical radiolucency of a tooth?
The periapical radiolucency is classically juxtapositioned to the apex of a tooth, which has a large carious lesion or large restoration or is fractured and/or is unresponsive to vitality testing, suggesting pulpal necrosis.
What is the effect of radiolucency on teeth?
The effect of the radiolucency on the adjacent teeth or anatomical structures is important. This effect is manifested by either displacement or erosion. The latter when applied to teeth, particularly their roots, is termed root resorption.
What is a radiolucency of the Crown of a tooth?
If the radiolucency is associated with the crown of an unerupted tooth, a dentigerous cyst or an odontogenic neoplasm (assuming a secondary relationship to it) should be considered. Lesions that commonly present as well-defined radiolucencies are cysts and neoplasms.
What is a radiolucency on an xray?
As alluded to above, a radiolucency shows up on an x-ray because the bone in that region is less dense (it contains less mineral content, or else there is an actual void in the bone tissue in that area). When dental x-rays are taken: Areas of high density show as white regions (referred to as radiopacities).
What causes Radiolucency in teeth?
Most of periapical radiolucencies are the result of inflammation such as pulpal disease due to infection or trauma. Not all radiolucencies near the tooth root are due to infection. Odontogenic or non odontogenic lesions can over impose the apices of teeth.
What does Radiolucency mean on xray?
(rā′dē-ō-lo͞o′sənt) adj. Allowing the passage of x-rays or other radiation; not radiopaque.
What does radiolucent mean in dentistry?
It is common to see dark areas, known as radiolucencies, on a dental x-ray. A radiolucency often represents a void or an area of tissue that is less dense. Some of these radiolucencies are normal, such as those that represent openings in the jaw bone that allow certain nerves to enter and exit the jaw.
How long does it take for periapical Radiolucency to heal?
The average radiographic rate of repair was 3.2 mm2/mo. Less than 6 months after treatment, 17.6% of lesions demonstrated complete radiographic resolution, whereas 70.6% showed radiographic resolution at 12 months or longer.
Is the root canal radiolucent?
Of the 271,980 untreated teeth, 2% had periapical radiolucencies. The technical quality of root canal treatment was decried by most authors of the included studies. Conclusions: The prevalence of periapical radiolucency was very high, broadly equivalent to 1 radiolucency per patient.
Does root canal infection show up on xray?
In the majority of cases, you will notice some type of symptom that indicates an infected root canal. Although, there are cases where there are no symptoms and the infection will only be found by your dentist on an x-ray.
How would you describe Radiolucency?
radiolucent. [ rā′dē-ō-lōō′sənt ] adj. Characterized by allowing passage of x-rays or other radiation; not radiopaque.
What is an example of radiolucent?
For example, on typical radiographs, bones look white or light gray (radiopaque), whereas muscle and skin look black or dark gray, being mostly invisible (radiolucent).
What appears radiolucent on a dental radiograph?
Structures that are cavities, depressions or openings in bone such as a sinus, fossa, canal or foramen will allow x-rays to penetrate through them and expose the receptor. These areas will appear radiolucent or black on radiographic images.
How is apical Radiolucency treated?
A large periapical radiolucency, as a result of pulp necrosis due to a persistent infection, might be believed to be refractory to conventional root canal treatment and considered a cyst and requires endodontic surgery (144).
How long does it take for bone to grow back after root canal?
An infection in the root canal often causes bone loss in the area near the root. In most cases, removing the infection from the root canal space allows the surrounding bone tissue to regenerate. It takes several months to a year for bone tissue to heal.
What causes a lesion on tooth root?
Periapical periodontitis or apical periodontitis (AP) is an acute or chronic inflammatory lesion around the apex of a tooth root, most commonly caused by bacterial invasion of the pulp of the tooth.
What is the medical term for radiolucent?
Radiolucent: Permeable to one or another form of radiation, such as X-rays. Radiolucent objects do not block radiation but let it pass. Plastic is usually radiolucent. The opposite of radiolucent is radiopaque.
What is an example of radiolucent?
For example, on typical radiographs, bones look white or light gray (radiopaque), whereas muscle and skin look black or dark gray, being mostly invisible (radiolucent).
What are radiolucent lines?
Radiolucent lines (RLLs) are defined as radiolucent intervals (measured in millimetres) between the cement and the bone [9]. The appearance of peripheral RLLs under the tibial component is a frequent occurrence in the immediate postoperative phase.
Are lungs radiolucent?
The air-filled lungs are the easiest penetrated and absorb the least amount of the beam - they are considered radiolucent. Bone is dense and absorbs more of the beam - they are considered radiopaque. Radiolucent tissues appear dark or black, radiopaque tissue appear light or white.
Why is my periapical radiolucency not visible?
It is usually triggered by bacterial invasion of the dental pulp and its presence is often an indication of poor oral health status. Also known as periradicular periodontitis or apical periodontitis, periapical radiolucency may not be easily detected by X-rays and could persist even after many treatments.
How to treat radiolucency in the periapical?
Management Of Periapical Radiolucency. The first option when it comes to dealing with this dental condition is through pulp therapy. If this is found to be insufficient, endodontic surgery is recommended to eliminate the disease. This is because surgery offers the dental surgeon immediate access to your root apex.
What are the symptoms of periapical radiolucency?
Clinical symptoms of periapical radiolucency include tenderness, pain, and swelling in varying degrees. It is imperative, however, that proper vitality tests are carried out to map out the patient’s symptoms if an appropriate diagnosis is to be made.
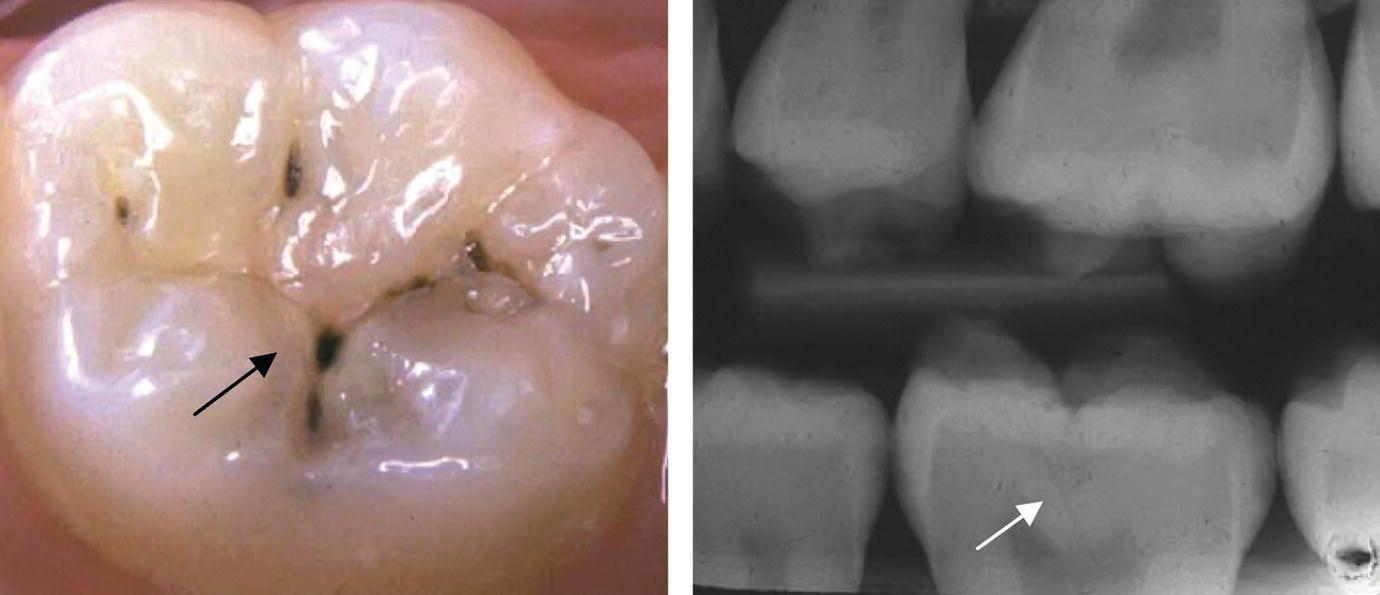
How to tell if a carious lesion is a carious lesion?
The earliest indication of an emerging carious lesion is marked by the appearance of a white, chalky spot on the tooth surface. This is an indication of enamel demineralization. There might be tissue destruction depending on how far the lesion has progressed.
What is periapical radiolucency?
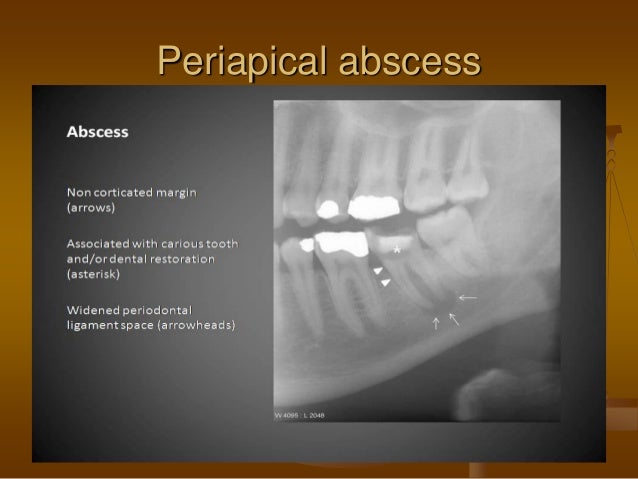
Periapical radiolucency is the descriptive term for radiographic changes which are most often due to apical periodontitis and radicular cysts, that is, inflammatory bone lesions around the apex of the tooth which develop if bacteria are spread from the oral cavity through a caries-affected tooth with necrotic dental pulp.1,2Clinical signs and symptoms such as pain, tenderness, and swelling may occur in varying degrees, depending on the diagnosis.3
How old was the average patient in the periapical radiolucency study?
A total of 110 patients participated in the study. Their mean age was 59 years (range 39–82 years), and 76% were men. Their demographic and clinical characteristics in relation to the presence of periapical radiolucency status are presented in Table 1.
What is the periapical status of each tooth?
The periapical status of each tooth was assessed at 0 for normal: the periapical periodontal ligament space and the surrounding bone showed no alteration – and 1 for periapical radiolucency: the presence of radiolucency or widening of the periapical periodontal ligament space to more than twice the normal width.16
Is periapical radiolucency a clinical problem?
Periapical radiolucency is often present as an element of poor oral health status and likely has an adverse clinical significance, which should motivate diagnostic and clinical attention to the findings.
Can cirrhosis cause radiolucency?
Infection as a complication of cirrhosis is a frequent cause of increased morbidity and mortality.11,12Periapical radiolucency due to apical periodontitis may contribute to this problem as it has been reported that apical periodontitis can precipitate a systemic inflammation activation in both healthy persons and patients with a variety of diseases.13,14However, it remains unknown whether this is also true for cirrhosis patients.
What is a lucency around the tooth root?from pubs.rsna.org
Myriad non-odontogenic lesions, both benign and malignant, may be seen as a lucency around the tooth root that mimics a periapical lucency due to apical periodontal or pulpal disease. These conditions include fissural cysts, cemento-osseous dysplasias, giant cell granulomata, and simple bone cysts.
What is the cavity in Figure 3?from pubs.rsna.org
Figure 3 Cavity and periapical lucency (granuloma). Sagittal CT image demonstrates a large cavity (*) in the crown of a second mandibular molar, involving both enamel and dentin. Widening of the periodontal ligament (arrow) around the apex of the tooth is seen, consistent with apical periodontitis. Sclerosis of the bone surrounding the infected tooth suggests chronic inflammation.
Why is it important to identify odontogenic sinus infection?from pubs.rsna.org
Identification of an odontogenic source of sinus infection is important because the pathophysiology, microbiology, and management differ from those for sinusitis originating within the sinus itself ( 20, 26 ). CT findings in odontogenic sinusitis may be identical to those for “typical” sinusitis, but they are more often unilateral. Odontogenic sinusitis may mimic focal mucosal thickening or a mucus retention cyst. The combination of findings related to apical periodontal disease and periapical abscess and the presence of a defect in the sinus floor are highly suspicious for a causal relationship ( Fig 9) ( 20, 27, 28 ).
What is periapical lucency?from pubs.rsna.org
Periapical lucency is often seen incidentally at head and neck imaging studies performed for indications not related to the teeth but may represent the cause of a patient’s symptoms. According to one study, 78% of periapical lesions are the result of an infectious or inflammatory process, usually due to apical periodontal or pulpal disease ( 1 ). Recognition of the typical radiologic features of apical periodontal disease results in early referral and proper treatment. Inadequate treatment of disease related to the teeth may result in complications and contribute to increased patient morbidity and health care costs ( 2, 3 ).
Why do you need root canals?from pubs.rsna.org
Root canals are performed in the setting of periapical lucency due to apical periodontitis and, together with antibiotics, are aimed at eliminating infection. If treatment is successful, bone regeneration and healing of the periapical lesion will ensue and manifest as a gradual reduction in lesion size.
Why does tooth decay happen?from montanapetdental.com
Why does this happen? When a tooth becomes non-vital (dies), whether or not they are infected, the necrotic pulp tissue begins to break down inside the tooth. Some of this material begins to leak out around the apex of the root through the small apical delta canals that extend from the end of the root canal to the outside of the root. If you look below at the final X-ray from the past newsletter, you can see the cement highlighting some of those canals, leading to the puff of cement (arrow) on the X-ray. As these materials leak outside the root, they elicit an inflammatory response in the periapical tissues. The presence of bacteria hastens this process. The end result is demineralization of the bone secondary to chronic inflammation.
Why is my periapical radiolucency not visible?from dentaldorks.com
It is usually triggered by bacterial invasion of the dental pulp and its presence is often an indication of poor oral health status. Also known as periradicular periodontitis or apical periodontitis, periapical radiolucency may not be easily detected by X-rays and could persist even after many treatments.
What is the difference between tooth No. 18 and 20?
tooth No. 20. Tooth No. 18 had previously treated root canals with a cast metal post extending into the distal root, while tooth No. 20 did not have previous endodontic treatment. A large (~15 mm in diameter, see PA
How can an endodontist control the outcome of his treatment?
One of the ways that the endodontist can control a more positive outcome of his treatment is to place the core buildup after completing the endodontic treatment, under rubber dam isolation. This will eliminate one of the links that may lead to failure of the treatment.
Can teeth be saved?
That teeth that would otherwise be extracted can be saved
What is the clinical history of tooth 19?
Clinical findings and dental history#N#The patient had a crown on tooth No. 19, which according to the patient, was placed 5 years prior. She had composite and amalgam restorations on her remaining maxillary and mandibular premolar and molar teeth in the quadrant. The patient did not have any intraoral swelling but had been experiencing dull pain on the tooth for some time. However, she had been too busy to have the problem evaluated earlier. Both teeth No. 18 and No. 20 responded normally to cold sensitivity testing. Probing depths were within normal limits, measuring 2 mm-3 mm as probed at eight different sites around the tooth, using the “walking-the-probe technique.”
How long did calcium hydroxide stay in the mesial canal?
Calcium hydroxide was again placed in the mesial canals for 3 more months, and completion of the treatment was planned for the next visit. It was now 1 year since the initiation of the retreatment. The healing of the furcal bone was phenomenal. Both the operator and the patient were very pleased with the results.
Can a dentist be faulted for a tooth loss?
And although neither the general dentist nor the oral surgeon can be faulted for the treatment that was about to be rendered, publication of these types of treatment results allow for the consideration of the possibility of retaining these teeth with long-term endodontic treatment.