What is a good score on the Morse fall scale?
Scores below 25 indicate a low fall risk, scores between 25 and 45 indicate a moderate risk whilst scores above 45 suggest the patient is at a high fall risk. Jump to: 1. Morse fall scale calculator. 2. Fall risk factors. 3. Morse scale scoring.
How is the fall risk scale used to identify risk factors?
Background: This tool can be used to identify risk factors for falls in hospitalized patients. The total score may be used to predict future falls, but it is more important to identify risk factors using the scale and then plan care to address those risk factors. Reference: Adapted from Morse JM, Morse RM, Tylko SJ.
What is a secondary diagnosis of fall risk?
■ If the patient has a secondary diagnosis, meaning 2 or more diagnoses in the patient chart, the risk of fall increases. ■ Ambulatory aid refers to the patient making use of walking aid (cane, crutches or wheelchair). ■ Intravenous therapy/ heparin lock checks whether the patient is under IV medication.
Can the total score be used to predict future falls?
The total score may be used to predict future falls, but it is more important to identify risk factors using the scale and then plan care to address those risk factors. Reference: Adapted from Morse JM, Morse RM, Tylko SJ. Development of a scale to identify the fall-prone patient.
What does presence of secondary diagnosis mean?
The secondary diagnosis refers to a coexisting condition that might exist at the time of patient admission. This condition might evolve over the course of the patient's stay, or it might be cause for further treatment.
What is high risk on Morse Fall Scale?
A patient who scores under 25 points is considered to be at low risk of falling, a patient who scores between 25–45 points is considered to be at moderate risk of falling, and a patient who scores higher than 45 points is considered to be at high risk of falling.
What are the components of the Morse fall risk scale?
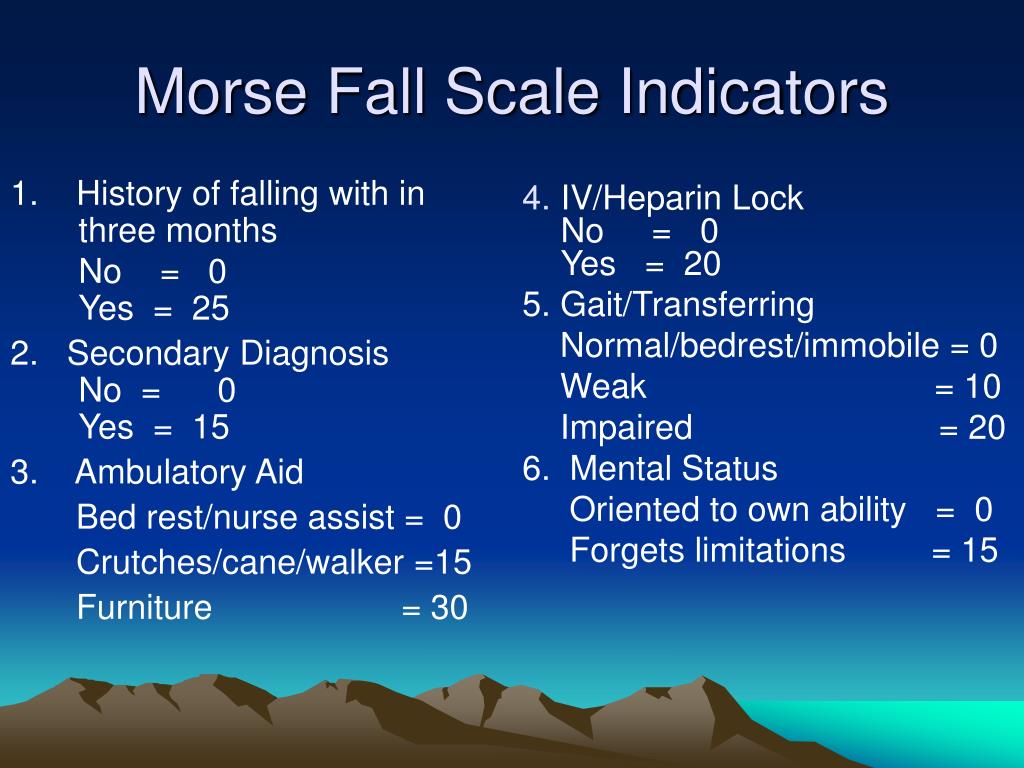
It involves the scoring of six items: fall history, presence of a secondary diagnosis, use of an ambulatory aid, use of an intravenous apparatus or heparin lock, impaired gait, and impaired mental status.
What is the purpose of the Morse Fall Scale and identify indicators that a patient is at risk for a fall?
Background: This tool can be used to identify risk factors for falls in hospitalized patients. The total score may be used to predict future falls, but it is more important to identify risk factors using the scale and then plan care to address those risk factors.
What are the secondary diagnosis for fall risk?
Secondary Diagnosis: • Consider factors which may increase risk for falls: illness/ medication timing and side effects such as dizziness, frequent urination, unsteadiness. IV or Hep Lock Present: • Implement toileting/rounding schedule. Instruct patient to call for help with toileting.
What is a bad fall risk score?
Score 0–125. 0–20 No risk or low risk; ≥25 Medium risk; ≥45, 50–55 High risk.
What are the differential diagnosis for falls?
The differential diagnosis of falls is very broad....Differential diagnosis.GeneralMechanical (e.g. poor footwear/visual impairment) PolypharmacyNeurologicalStroke Peripheral neuropathyGenitourinaryIncontinence Urinary tract infectionEndocrineHypoglycaemiaMusculoskeletalArthritis Disuse atrophy2 more rows•Jun 14, 2022
How is Morse Fall Scale scored?
This is scored as 25 if the patient has fallen during the present hospital admission or if there was an immediate history of physiological falls, such as from seizures or an impaired gait prior to admission. If the patient has not fallen, this is scored 0.
What are the 2 main risk factors involved in falls?
Common risk factors for falls limitations in mobility and undertaking the activities of daily living. impaired walking patterns (gait)
What is a nursing diagnosis for fall risk?
A widely accepted definition is “an unplanned descent to the floor with or without injury to the patient.” The nursing diagnosis for risk of falls is “increased susceptibility to falling that may cause physical harm.”
What are the 5 key steps in a falls risk assessment?
You can do it yourself or appoint a competent person to help you.Identify hazards.Assess the risks.Control the risks.Record your findings.Review the controls.
What does the Morse scale measure?
Predicts risk of falling based on personal fall history, mental status and other risk factors. In the text below the calculator there is more information on patient parameters used, scoring method and about the original study.
What does high fall risk mean?
High Fall Risk - Implement High Fall Risk interventions per protocol. History of more than one fall within 6 months before admission. Patient has experienced a fall during this hospitalization. Patient is deemed high fall-risk per protocol (e.g., seizure precautions)
What are the fall risk categories?
Assigning fall risk categories (high, moderate and low) based on the numerical score of a fall risk assessment alone may not always be clinically useful or appropriate.
How is Weight risk scored?
The risk is multiplied by the weight, and then added to the other risks multiplied by their weights. The calculated risk can be produced by the summation of each risk multiplied by its weight, and divided by the total weight of all risks.
Which patient activity has the highest risk for falls?
According to a study supported by the Agency for Healthcare Research and Quality , many falls in hospital happen when the patient is alone or involved in elimination-related activities (for example, walking to or from the bathroom or bedside commode, reaching for toilet tissue, or exiting a soiled bed).
What is Morse fall scale?
This Morse fall scale calculator aims to screen fall risk in all hospitalized patients and recommends the initiation of fall prevention procedures where adequate. There is more information on the risk factors involved in this fall screening tool available below the form.
How does this Morse fall scale calculator work?
This health tool evaluates the risk of falling in hospitalized patients based on certain patient status related variables.
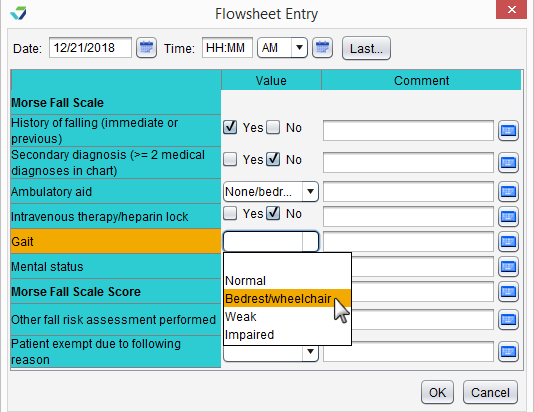
What is the difference between impaired and weak gait?
Gait – evaluates the presentation of the patient and their balance status. Weak gait is defined as short steps, the patient in a stooped state but able to lift head, seeking support from furniture while walking but just for reassurance. Impaired gait is defined as short steps with shuffle, head down, difficult arising from chair, impaired balance or needing walking aid.
What is secondary diagnosis?
Secondary diagnosis (2 or more medical diagnoses in chart) – evaluates the existence of other comorbidities.
How is mental status evaluated?
Mental status – evaluated through the ability of the patient to assess their own condition and the consistency of their answers. Once the risk factors are highlighted and the medical professional has an idea about the risk category the patient is in, they can devise a care plan oriented toward prevention.
Who developed the fall prone scale?
1) Morse JM, Morse RM, Tylko SJ. (1989) Development of a scale to identify the fall-prone patient. Can J Aging; 8:366-7.
Should fall prevention interventions be activated in patients with high risk?
In the cases of patients deemed low risk, the advice is to continue with basic nursing care, in patients with moderate risk, the standard fall prevention interventions should be activated while in patients with high risk, the high risk fall prevention intervention should prevail.
When is Morse fall scale administered?
Often, the Morse fall scale is administered in conjunction with other tests, during clinical examinations and during reviews of current therapy.
Why is Morse fall scale used?
The Morse fall scale can be used to screen the patients that need to be targeted with prevention strategies.
What does a fall risk score of 25 mean?
Scores below 25 indicate a low fall risk, scores between 25 and 45 indicate a moderate risk whilst scores above 45 suggest the patient is at a high fall risk.
What is Morse scale?
The Morse fall scale screens elderly patients for risk of falling to help the initiation of fall prevention measures.
When did Morse and al. conduct a study on the morbidity and mortality of the elderly patient?
Morse et al. have conducted a study on the morbidity and mortality of the elderly patient, in 1989 , with specific interest into patient falls.
How many fall risk parameters are there in the fall risk tool?
The tool consists of 6 fall risk parameters:
