What is the “gold standard” for monitoring ICP?
What is the "gold standard" for monitoring ICP? ventriculostomy, because it directly measures the pressure in the ventricles, facilitates removal/sampling of CSF, and allows for intracranial drug administration What is the major complication associated with ventriculostomy?
What is normal intracranial pressure (ICP)?
Intracranial Pressure Monitoring - StatPearls - NCBI Bookshelf The normal intracranial pressure (ICP) ranges within 7 to 15 mm Hg while in the vertical position, it does not exceed −15 mm Hg.
How is intracranial pressure (ICC) measured?
Another important aspect of measuring ICP is securing the pressure–volume buffering or reserve capacity, which is more commonly referred to as intracranial compliance (ICC). The pressure–volume curve (Fig. 1) describes the relationship between change in ICP and change in volume of the intracranial constituents (e.g. blood, CSF or a mass).
What is the history of intracranial pressure (ICP) monitoring?
In 1891, Heinrich Quincke [ 11] was the first to indirectly measure ICP, or lumbar cerebrospinal fluid (CSF) pressure, via lumbar puncture, but it took more than half a century before ICP monitoring was introduced in clinical practice.

Which ICP monitoring method is the most accurate?
intraventricular catheterICP is the pressure in the skull. The intraventricular catheter is the most accurate monitoring method.
How is the intracranial pressure measured?
Intracranial pressure (ICP) monitoring is a diagnostic test that helps your doctors determine if high or low cerebrospinal fluid (CSF) pressure is causing your symptoms. The test measures the pressure in your head directly using a small pressure-sensitive probe that is inserted through the skull.
Which procedure is considered the gold standard for managing ICP?
An intraventricular drain connected to an external pressure transducer is still considered to be “golden standard” method. ICP can be controlled by CSF drainage and the transducer may be zeroed externally.
What is the instrument used to measure intracranial pressure called?
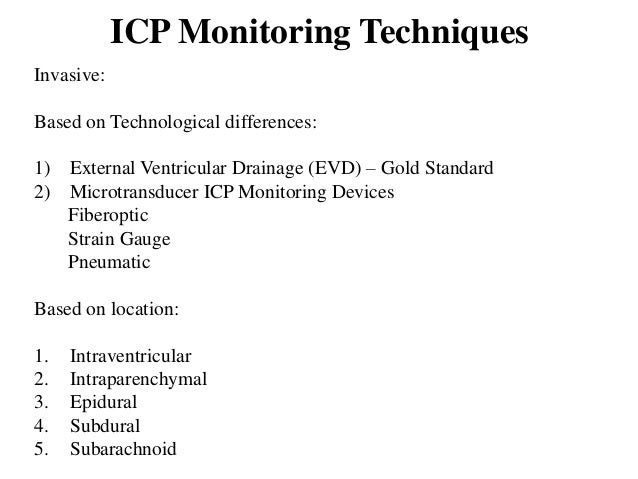
The three main types of ICP monitor are the External Ventricular Drain (EVD), the Subarachnoid Bolt, and the Epidural bolt (Fig. 2). These probes can often also be used to measure other physiological parameters, including temperature, lactate, and pH.
What is the most important indicator of increased ICP?
Measurement of Opening Pressure with a Lumbar Puncture A measurement greater than 20 mm Hg is suggestive of raised ICP. Brain imaging should precede an LP because LP can cause a sudden and rapid decrease in ICP and the sudden change in volume can lead to herniation. Several devices can be used for ICP monitoring.
How is non invasive ICP measured?
Quantitative assessment of ICP can be made noninvasively in two different ways: by measuring changes in diameter of the optic nerve sheath with an appropriate technique (ultrasound or MRI), or by using ophthalmodynamometry to determine the pressure in the central retinal vein, which is normally slightly higher (1- ...
How is cerebrospinal fluid pressure measured?
Your surgeon inserts a catheter (flexible tube) through the needle, the removes the needle, leaving the catheter in place. The catheter is gently bandaged to the skin on your lower back, then connected to a device that measures the CSF pressure over a 24- to 72-hour period.
Does an EVD measure ICP?
There are two types of ICP monitoring, a direct ICP monitor (Codman™) or via an EVD. An ICP monitor is utilized when ICP monitoring is needed without the need to drain CSF, e.g. investigation of headache.
What is a Codman monitor?
The Codman MicrosensorTM measures intracranial pressure via a strain gauge microchip located at the tip of the catheter. Pressure is reflected as an electrical voltage that is transmitted to the proximal end of the catheter through nylon encapsulated copper wires.
Which device is used for monitoring a patient's neurological status of brain function?
Electroencephalography, or EEG, monitors the brain's electrical activity through the skull.
What is the normal intracranial pressure?
The normal intracranial pressure (ICP) ranges within 7 to 15 mm Hg while in the vertical position, it does not exceed −15 mm Hg. Overnight sleep monitoring is considered the “gold standard” in conscious patients. [1]
What level of ICP monitoring is recommended?
ICP monitoring is also recommended (Level III recommendations) in: [8]
What monitors are used for ICP?
Currently, intraventricular monitor with the aid of ventriculostomy or the use of intraparenchymal strain gauge or fiber optic monitors is the recommendation for ICP monitoring. So appropriate monitoring devices should be available. There needs to be utmost care for strict adherence to aseptic conditions during these procedures. There also is paramount importance of implementing algorithmic management guidelines in all patients with invasive ICP monitors for safeguarding all monitor sets.
What is a decompressive craniectomy?
A decompressive craniectomy performed as a last resort for intracranial hypertension refractory to medical management
How many peaks are there in a pulse waveform?
The pulse component of the waveform shows three peaks:
Which is more accurate, a strain gauge or fiber optic based system inserted into the ventricles or brain?
Strain gauge or fiber optic based systems inserted into the ventricles or brain parenchymas are more accurate compared to fluid-coupled or pneumatic devices.
Can a slit ventricle complicate ICP?
Difficulties in catheter placement in cases of severe brain edema with slit ventricles can complicate intraventricular monitoring of ICP.
What is intracranial pressure monitoring?
Intracranial pressure monitoring (ICP) is based on the doctrine proposed by Monroe and Kellie centuries ago. With the advancement of technology and science, various invasive and non-invasive modalities of monitoring ICP continue to be developed. An ideal monitor to track ICP should be easy to use, accurate, reliable, reproducible, inexpensive and should not be associated with infection or haemorrhagic complications. Although the transducers connected to the extra ventricular drainage continue to be Gold Standard, its association with the likelihood of infection and haemorrhage have led to the search for alternate non-invasive methods of monitoring ICP. While Camino transducers, Strain gauge micro transducer based ICP monitoring devices and the Spiegelberg ICP monitor are the emerging technology in invasive ICP monitoring, optic nerve sheath diameter measurement, venous opthalmodynamometry, tympanic membrane displacement, tissue resonance analysis, tonometry, acoustoelasticity, distortion-product oto-acoustic emissions, trans cranial doppler, electro encephalogram, near infra-red spectroscopy, pupillometry, anterior fontanelle pressure monitoring, skull elasticity, jugular bulb monitoring, visual evoked response and radiological based assessment of ICP are the non-invasive methods which are assessed against the gold standard.
Is invasive ICP monitoring necessary?
Traumatic brain injury frequently causes an elevation of intracranial pressure (ICP) that could lead to reduction of cerebral perfusion pressure and cause brain ischemia. Invasive ICP monitoring is recommended by international guidelines, in order to reduce the incidence of secondary brain injury; although rare, the complications related to ICP probes could be dependent on the duration of monitoring. The aim of this manuscript is to clarify the appropriate timing for removal and management of invasive ICP monitoring, in order to reduce the risk of related complications and guarantee adequate cerebral autoregulatory control. There is no universal consensus concerning the duration of invasive ICP monitoring and its related complications, although the pertinent literature seems to show that the longer is the monitoring maintenance, the higher is the risk of technical issues. Besides, upon 72 h of normal ICP values or less than 72 h if the first computed tomography scan is normal (none or minimal signs of injury) and the neurological exam is available (allowing to observe variations and possible occurrence of new-onset pathological response), the removal of invasive ICP monitoring can be justified. The availability of non-invasive monitoring systems should be considered to follow up patients' clinical course after invasive ICP probe removal or for substituting the invasive monitoring in case of contraindication to its placement. Recently, optic nerve sheath diameter and straight sinus systolic flow velocity evaluation through ultrasound methods showed a good correlation with ICP values, demonstrating their potential role in place of invasive monitoring or in the early weaning phase from the invasive ICP monitoring.
What is the importance of intracranial pressure?
Elevated intracranial pressure (ICP) is an important cause of secondary brain injury, and a measurement of ICP is often of crucial value in neurosurgical and neurological patients.
Is noninvasive monitoring accurate?
The noninvasive methods have many advantages, but remain less accurate compared with the invasive techniques. None of the noninvasive techniques available today are suitable for continuous monitoring, and they cannot be used as a substitute for invasive monitoring.
Can ICP be used as a screening method?
They can , however, provide a reliable measurement of the ICP and be useful as screening methods in select patients , especially when invasive monitoring is contraindicated or unavailable.
Is intraparenchymal ICP monitoring safe?
Intraparenchymal ICP monitoring methods are considered to be a safer alternative but can, in certain conditions, be imprecise due to zero drift and still require an invasive procedure. An accurate noninvasive method to measure elevated ICP would therefore be desirable.
How is ICP treated?
Increased intracranial pressure is an emergency. Treatment might include:
How do you know if you have an ICP?
These are the most common symptoms of an ICP: Headache. Blurred vision. Feeling less alert than usual. Vomiting. Changes in your behavior. Weakness or problems with moving or talking. Lack of energy or sleepiness. The symptoms of ICP may look like other conditions or medical problems.
What causes ICP?
Too much cerebrospinal fluid ( the fluid around your brain and spinal cord)
Is intracranial pressure dangerous?
Key points about increased intracranial pressure (ICP) ICP is a dangerous condition. It is an emergency and requires immediate medical attention. Increased intracranial pressure from bleeding in the brain, a tumor, stroke, aneurysm, high blood pressure, brain infection, etc. can cause a headache and other symptoms.
Can ICP be prevented?
You can reduce your risk of certain underlying conditions that may lead to ICP such as high blood pressure, stroke or infection. If you have any of the symptoms, get medical attention immediately.
What is the term for an increase in the three components of the skull?
an increase in any of the three components of the skull (blood, brain tissue, CSF), like a lesion (hematoma, abcess, contusion, tumor), cerebral edema (tumors, hydrocephalus, head injury or brain inflammation), or metabolic insult, brought about by MVA, stroke,
Where can a pressure transducer be used?
Can be measured in the ventricles, subarachnid space, epidural space, or brain tissue using a pressure transducer
What should a PTS take for GI bleeding?
watch for hyperglycemia, increased incidence of infections, and GI bleeding; monitor fluid intake and sodium and glucose levels regularly (q 6 hours), pts should also be getting antacids or histamine H2 receptor blockers or proton pump inhibitors to prevent GI ulcers and bleeding
What is Cushing's triad?
Cushing's Triad, temperature alterations related to impact on hypothalamus
What is the normal intracranial pressure?
The normal range for intracranial pressure (ICP) is 5 – 15mmHg. The average intracranial volume is 1700ml (composed of the brain 1400ml + CSF 150ml + blood 150ml), with Cerebrospinal Fluid (CSF) production around 500 – 600ml per day.
What is ICP monitoring?
Whilst ICP monitoring is most commonly used for the management of severe head trauma, its use also extends to CSF circulatory disorders, and can be either diagnostic or therapeutic (by removing CSF to reduce pressures).
What are the different types of ICP monitors?
The three main types of ICP monitor are the External Ventricular Drain (EV D), the Subarachnoid Bolt , and the Epidural bolt (Fig. 2).
How is cerebral perfusion pressure calculated?
The brain can autoregulate blood flow, through cerebral vessel constriction or dilatation, in order to ensure constant flow isolated from fluctuations in systemic blood pressure*; the Cerebral Perfusion Pressure is calculated by Mean Arterial Pressure minus Intracranial Pressure.
What is the purpose of the waveforms produced from ICP monitoring?
The waveforms produced from the ICP monitoring can be used to infer the underlying pathology present. The wave forms produced are summarised in Table 1.
What is the primary protection of the brain?
In order to protect the brain, the blood and CSF volume can be comprised as the primary protection. However, this mechanism can be overcome with large increases to these volumes.
How to measure pressure in a CSF?
Attach the catheter to non-pressurised tubing filled with saline solution and connected to non-flush strain-gauge transducer (this will measure the pressure transmitted from CSF in the ventricles). Level the transducer to zero.
How to measure ICP?
The most widespread use of measuring ICP is via lumbar puncture (LP) and involves advancing a needle into the lumbar intrathecal space, which is linked on the other end to an external pressure transducer. The common way is to measure fluid level as centimeters of water (H 2 O) and use this as an indication of ICP. A requirement for this measurement methodology to provide relevant results is obstruction-free CSF communication pathways. Estimating ICP from LP is common in neurological practice, and is widely used for assessing ICP in individuals with idiopathic intracranial hypertension (IIH) events, although the limitations involved in estimating ICP by LP are well known [ 136 ].
Who first measured ICP?
In 1891, Heinrich Quincke [ 11] was the first to indirectly measure ICP, or lumbar cerebrospinal fluid (CSF) pressure, via lumbar puncture, but it took more than half a century before ICP monitoring was introduced in clinical practice. The year 2020 marks 70 years since Pierre Janny, in France, published his thesis on ICP monitoring [ 12] and 60 years since Nils Lundberg, in Sweden, presented his [ 13 ]. Lundberg’s work on measurements of ICP via ventricular puncture was instrumental in establishing ICP as a clinical tool. Many still consider measuring ICP using fluid-filled systems via ventricular catheters as the gold standard.
What is intracranial disease?
Intracranial disease processes and pathophysiological events after e.g. injuries or bleeds , involve complex cascades of events beyond alterations in ICP. The ICP primarily refers to the pressure and pressure–volume reserve within the skull, and therefore describes only part of the pathophysiological cascades. For this reason, monitoring of several physiological variables (e.g. CBF, brain oxygenation and metabolism), referred to as multi-modality monitoring, has been advocated [ 9, 38 ]. Through this type of monitoring, ICP can be measured along with other parameters such as brain tissue oxygenation (PbtO 2 ), temperature, cerebral blood flow velocity, cerebral metabolism (micro-dialysis), and assessment of electro cortical activity. The multi-modality approach allows for incorporation of different aspects of the brain state in patient surveillance and can contribute to a more holistic view of the patient’s condition. Catheters for multi-parametric measurements, intended for neuro-intensive care, have therefore appeared on the market. The Neurovent-PTO (Raumedic) is one example of an integrated catheter that allows for simultaneous measurements of ICP, temperature and tissue oxygen (O 2) [ 39 ].
How to obtain reliable data from preclinical studies of ICP?
Preferably, preclinical studies should sample the continuous raw ICP signals and include assessment of both the static and pulsatile ICP after single wave assessment so as to ensure correct pressure assessments. However, in freely moving animals, high signal-to-noise ratio is expected.
What is the difference between pulsatile and static ICP?
Measurements of static versus pulsatile ICP. The static ICP (mean ICP) is an absolute pressure value measured against a reference pressure (here illustrated by the green line), not considering the pressure changes occurring during the cardiac cycle. The pulsatile ICP is the pulse pressure or the pressure changes occurring during the cardiac cycle (here illustrated by the blue line). A single ICP wave is characterized by an increase in pressure from diastolic minimum pressure to systolic maximum pressure (the peaks are illustrated by the red dots). The single ICP wave amplitude is the peak-to-peak pressure difference. Illustration: Øystein Horgmo, University of Oslo
What is intracranial volume curve?
The intracranial pressure–volume curve. There is a non-linear relationship between change in intracranial pressure (ICP) and intracranial volume (Volume). At the flat portion of the curve, the pressure–volume reserve or buffering capacity is good (i.e. the intracranial compartment accepts a rather large change in intracranial volume without resulting in increased ICP). This implies that intracranial elastance is low (intracranial compliance is high). At the vertical portion of the curve, a small change in intracranial volume causes a marked rise in ICP; pressure–volume reserve capacity is low (high intracranial elastance or low intracranial compliance). The pressure–volume curve was established from measuring mean ICP. In the context of pulsatile ICP, at the flat portion of the curve the net intracranial blood volume change during the cardiac beat (about 1 ml) causes a small single wave amplitude (< 3–4 mmHg). At the vertical portion of the curve, the same net intracranial blood volume change during the cardiac beat (about 1 ml) results in a much larger ICP wave amplitude (> 4–5 mmHg).
Why has ICP not moved further?
One reason why the field has not moved further is limited awareness of the constraints and weaknesses of the current ICP measurement approaches. Clinical practice and scientific reporting is thereby hampered by uncertainty about the ICP scores. In this critical review, we have addressed two areas in particular: the role of ICP source signal control and the impact of reference pressure variability on static ICP scores. For a number of reasons, these issues have received less attention in the past, not least because ICP monitoring systems provide limited opportunities for exploring these methodological weaknesses. In our opinion, the major issue with today’s practice is lack of signal quality control. As long as these issues remain largely unexplored, they cannot be defined as clinically irrelevant. All issues that may erroneously alter the ICP scores provided to health care personnel are important, as incorrect ICP scores can result in wrong treatment. These aspects deserve greater examination from the ICP community. The field of ICP measurements needs to take a step from analog to digital technology.