How long does it take staph infection to heal?
The healing of staph infections may vary depending on the type of the infection. For example, a boil may take anywhere between 10-20 days to heal completely. Availing treatment may speed its healing.
What happens if staph infection is untreated?
What are the symptoms of MRSA?
- Skin. An MRSA skin infection is sometimes mistaken for a large pimple, impetigo, or spider bite due to their similar appearance.
- Lungs. MRSA can cause severe pneumonia if it gets into your lungs. ...
- Heart. MRSA can infect the inside of your heart. ...
- Bloodstream. Bacteremia means there are bacteria in your bloodstream. ...
- Bone. ...
What disease is caused produced by strptococcus?
Streptococcus pyogenes is the leading cause of uncomplicated bacterial pharyngitis and tonsillitis commonly referred to as strep throat. Acute diseases associated with Streptococcus pyogenes occur chiefly in the respiratory tract (sinusitis, otitis), bloodstream (sepsis, endocarditis, meningitis), or the skin (impetigo, cellulitis, necrotizing fasciitis, myositis}.
What are some diseases caused by Staphylococcus?
What are some diseases caused by Staphylococcus? Staphylococcus can cause diseases such as abscesses, impetigo, food poisoning, cellulitis, mastitis, scalded skin syndrome, and toxic shock syndrome. MRSA , or methicillin-resistant Staphylococcus aureus , is a type of Staph infection resistant to many different antibiotics.
See more
What illness does Staphylococcus aureus cause?
It is the leading cause of skin and soft tissue infections such as abscesses (boils), furuncles, and cellulitis. Although most staph infections are not serious, S. aureus can cause serious infections such as bloodstream infections, pneumonia, or bone and joint infections.
What is staphylococcal illness?
What is staphylococcal disease? Staphylococci are bacteria that can cause a variety of syndromes from skin infections and food poisoning, to severe invasive disease which can result in septicemia or death.
Why is Staphylococcus aureus so often implicated in food poisoning?
Causes for Staphylococcus aureus food poisoning aureus has a high salt tolerance, and can grow in ham and other meats, and in dairy products. The toxins that the bacteria produce are also heat resistant and cannot be destroyed through cooking. Once food has been contaminated, bacteria begin to multiply.
What is Staphylococcus infection caused by?
Staph infections are caused by staphylococcus bacteria. These types of germs are commonly found on the skin or in the nose of many healthy people. Most of the time, these bacteria cause no problems or cause relatively minor skin infections.
What are the symptoms of Staphylococcus aureus?
Skin: Most commonly, Staphylococcus aureus bacteria cause skin infection. This can produce boils, blisters, and redness on your skin. These infections can be anywhere on your body, including your face, often around your mouth and nose.
Is Staphylococcus aureus a foodborne illness?
Staph foodborne illness is a type of foodborne illness caused by infection with the Staphylococcus aureus (S. aureus) bacterium. The bacteria multiply in foods and produce toxins especially if food is kept at room temperature.
What toxins are produced by Staphylococcus aureus?
Amongst the more common toxins secreted by S. aureus are hemolysin, leukotoxin, exfoliative toxin, enterotoxin, and toxic-shock syndrome toxin-1 (TSST-1). Aside from toxins, staphylococcal virulence factors also include enzymes and surface proteins.
Which of the following food intoxication is caused by Staphylococcus aureus?
Staph food poisoning is a gastrointestinal illness caused by eating foods contaminated with toxins produced by the bacterium Staphylococcus aureus (Staph) bacteria.
What Is Staphylococcal Food Poisoning?
Staphylococcal food poisoning is a gastrointestinal illness caused by eating foods contaminated with toxins produced by the bacterium Staphylococcu...
How Do People Get Staphylococcal Food Poisoning?
People who carry Staph can contaminate food if they don’t wash their hands before touching it. Staph can also be found in unpasteurized milk and ch...
What Are The of Staphylococcal Food Poisoning?
Staphylococcal toxins are fast-acting, symptoms usually develop within 30 minutes to 6 hours. Patients typically experience vomiting, nausea, stoma...
How Do I Know If I Have Staphylococcal Food Poisoning?
Toxin-producing Staph can be identified in stool or vomit using specialized techniques. The toxins can also be detected in foods. Suspicion of stap...
How Is Staphylococcal Food Poisoning Treated?
For most patients, staphylococcal food poisoning is a brief illness. The most important treatment is plenty of fluids. Medicines may be given to de...
Are Sick Patients Contagious?
Patients with this illness are not contagious because the toxins are not transmitted from one person to another.
How Can Staphylococcal Food Poisoning Be ?
Staphylococcal food poisoning can be prevented by preventing the contamination of food with Staph. The following food safety tips(https://www.cdc.g...
Could Staphylococcal Toxins Be Used in A Bioterrorist Attack?
Staph toxins could be used as a biological agent either by contamination of food or water or by aerosolization (using pressure to produce a fine mi...
What happens if you eat staph?
If food is contaminated with Staph, the bacteria can multiply in the food and produce toxins that can make people ill. Staph bacteria are killed by cooking, but the toxins are not destroyed and will still be able to cause illness. Foods that are not cooked after handling, such as sliced meats, puddings, pastries, and sandwiches, ...
How long does it take for staph to kill you?
What are the symptoms of Staph food poisoning? Staph food poisoning is characterized by a sudden start of nausea, vomiting, and stomach cramps. Most people also have diarrhea. Symptoms usually develop within 30 minutes to 8 hours after eating or drinking an item containing Staph toxin, and last no longer than 1 day.
How to tell if you have staph?
What are the symptoms of Staph food poisoning? 1 Staph food poisoning is characterized by a sudden start of nausea, vomiting, and stomach cramps. Most people also have diarrhea. 2 Symptoms usually develop within 30 minutes to 8 hours after eating or drinking an item containing Staph toxin, and last no longer than 1 day. Severe illness is rare. 3 The illness cannot be passed from one person to another.
How many people have staph on their nose?
About 25% of people and animals have Staph on their skin and in their nose. It usually does not cause illness in healthy people, but Staph has the ability to make toxins that can cause food poisoning.
Can you detect staph in stool?
Although laboratory tests can detect toxin-producing Staph in stool, vomit, and foods, these tests are usually not ordered except during an outbreak.
What are the two conditions that allow staphylococcal food poisoning to occur?
For staphylococcal food poisoning to occur following the ingestion of a given food, two conditions are necessary. First, S. aureus has to be present in the food; second, foods stored at incorrect temperatures and time allow growth of this pathogen and the production of enterotoxin.
How to avoid S. aureus?
To avoid contaminating the food with S. aureus, handle and prepare food safely: Ensure raw foods of animal origin are obtained following good hygienic practices, to reduce the possibility of S. aureus contamination. Food handlers should use appropriate protective clothing (e.g. gloves) and thoroughly wash hands.
What foods are most likely to cause staphylococcal poisoning?
The foods that have been most frequently implicated in cases of staphylococcal food poisoning are poultry and cooked meat products such as ham or corned beef. Other foods implicated were milk and milk products, canned food and bakery products.
What is the most common cause of food poisoning?
Staphylocococcus aureus (food poisoning) Staphylococcal food poisoning is an acute intoxication that occurs when food contaminated with enterotoxin produced by this bacterium is consumed. Although precise data regarding the exact number of cases is lacking, staphylococcal food poisoning is considered to be among the most common causes ...
What temperature does S. aureus need to grow?
For example, it needs temperatures of between 7°C and 48°C to be able to grow, with an optimum temperature of 37°C.
How long does it take for a staph to go away?
Staphylococcal food poisoning is usually self-limiting, resolving within one or two days. In a small percentage of cases it can be more severe, especially in infants, the elderly and immunocompromised patients.
How long does it take for a fever to go away after exposure?
other symptoms may include mild fever, weakness, dizziness and chills. Symptoms usually start 1 to 10 hours after exposure and go away in 1 to 2 days . In some cases, the illness may be more severe. If you have serious symptoms, you should see your doctor.
What is the treatment for staph infection?
Treatment of Staph Infections. Antibiotics. Sometimes surgical removal of infected bone and/or foreign material. Infections due to Staphylococcus aureus are treated with antibiotics. Doctors try to determine whether the bacteria are resistant to antibiotics and, if so, to which antibiotics.
What is the most dangerous bacteria?
Staphylococcus aureus is the most dangerous of all of the many common staphylococcal bacteria. These gram-positive, sphere-shaped (coccal) bacteria (see figure How Bacteria Shape Up) often cause skin infections but can cause pneumonia, heart valve infections, and bone infections.
What is the name of the bacteria that are resistant to beta-lactam antibiotics?
Strains of bacteria that are resistant to almost all beta-lactam antibiotics are called methicillin-resistant Staphylococcus aureus (MRSA). Methicillin is a type of penicillin. MRSA strains are common when infection is acquired in a health care facility (called hospital-acquired infection). Some strains of MRSA cause infections ...
What antibiotics are used for heart grafts?
If an infection involves bone or foreign material in the body (such as heart pacemakers, artificial heart valves and joints, and blood vessel grafts), rifampin and possibly another antibiotic are sometimes added to the antibiotic regimen.
How do bacteria spread?
These bacteria are spread by having direct contact with an infected person, by using a contaminated object, or by inhaling infected droplets dispersed by sneezing or coughing. Skin infections are common, but the bacteria can spread through the bloodstream and infect distant organs.
What causes blisters on hands?
Skin infections may cause blisters, abscesses, and redness and swelling in the infected area. The diagnosis is based on the appearance of the skin or identification of the bacteria in a sample of the infected material. Thoroughly washing the hands can help prevent spread of infection.
Can you get MRSA outside of a hospital?
MRSA infection can be acquired outside of a health care facility. The community-acquired MRSA strains are usually susceptible to other antibiotics, such as trimethoprim/sulfamethoxazole, clindamycin, minocycline, or doxycycline, as well as to the antibiotics used to treat MRSA infections acquired in the hospital.
What are the diseases caused by S. aureus?
aureus can cause a range of illnesses, from minor skin infections, such as pimples, impetigo, boils, cellulitis, folliculitis, carbuncles, scalded skin syndrome, and abscesses, to life-threatening diseases such as pneumonia, meningitis, osteomyelitis, endocarditis, toxic shock syndrome, bacteremia, and sepsis.
Where is Staphylococcus aureus found?
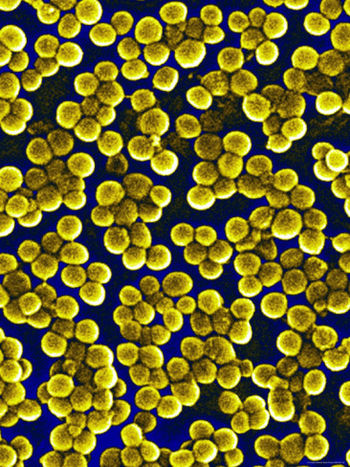
Staphylococcus aureus is a Gram-positive, round-shaped bacterium, a member of the Firmicutes, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin.
How many lineages does Staphylococcus aureus have?
Staphylococcus aureus can be sorted into ten dominant human lineages. There are numerous minor lineages as well, but these are not seen in the population as often. Genomes of bacteria within the same lineage are mostly conserved, with the exception of mobile genetic elements. Mobile genetic elements that are common in S. aureus include bacteriophages, pathogenicity islands, plasmids, transposons, and staphylococcal cassette chromosomes. These elements have enabled S. aureus to continually evolve and gain new traits. There is a great deal of genetic variation within the S. aureus species. A study by Fitzgerald et al. (2001) revealed that approximately 22% of the S. aureus genome is non-coding and thus can differ from bacterium to bacterium. An example of this difference is seen in the species' virulence. Only a few strains of S. aureus are associated with infections in humans. This demonstrates that there is a large range of infectious ability within the species.
How long does S. aureus last?
It is capable of generating toxins that produce food poisoning in the human body. Its incubation period lasts one to six hours, with the illness itself lasting from 30 minutes to 3 days. Preventive measures one can take to help prevent the spread of the disease include washing hands thoroughly with soap and water before preparing food. Stay away from any food if ill, and wear gloves if any open wounds occur on hands or wrists while preparing food. If storing food for longer than 2 hours, keep the food below 5 or above 63 °C.
How to prevent S. aureus?
Preventive measures include washing hands often with soap and making sure to bathe or shower daily. S. aureus is a significant cause of chronic biofilm infections on medical implants, and the repressor of toxins is part of the infection pathway. S. aureus can lay dormant in the body for years undetected.
What is the name of the bacterium that grows on blood agar plates?
In medical literature, the bacterium is often referred to as S. aureus, Staph aur eus or Staph a.. S. aureus appears as staphylococci (grape-like clusters) when viewed through a microscope, and has large, round, golden-yellow colonies, often with hemolysis, when grown on blood agar plates.
Where is S. aureus found?
In humans, S. aureus can be present in the upper respiratory tract, gut mucosa, and skin as a member of the normal microbiota. However, because S. aureus can cause disease under certain host and environmental conditions, it is characterized as a "pathobiont".
How does Staphylococcus aureus affect the body?
Epidemiology of Staphylococcus aureus. Staphylococcus aureus can cause illness by preformed toxin production as well as by infecting both local tissues and the systemic circulation. Disease transmission can occur in the following settings: Gastrointestinal: Staphylococcus aureus causes acute episodes of food poisoning via preformed enterotoxins.
What is the best treatment for Staphylococcus aureus?
Treatment. Staphylococcal aureus are susceptible to beta-lactamase resistant penicillins such as ticarcillin and pipercillin. Vancomycin is the drug of choice for MRSA infections.
What is the MRSA strain?
Nosocomial infections: Methicillin resistant Staphylococcal aureus (MRSA) is a strain of the bacteria that is commonly implicated in nosocomial infections.
What is S. aureus?
S. aureus is also responsible for many infective and systemic infections in the health care setting (nosocomial infections).
How long does it take for a staph infection to incubate?
Incubation Period for foodborne Staphylococcal aureus disease is 1-6 hours. Diagnosis Staphylococcal aureus gastrointestinal illness can be diagnosed by isolating the preformed toxins from the contaminated food item. Systemic infections are best diagnosed by blood cultures.
What foods are susceptible to staphylococcus?
Food items likely to be infected by staphylococcal food poisoning include meat and meat products; poultry and egg products; salads such as egg, tuna, chicken, potato, and macaroni; bakery products such as cream-filled pastries, cream pies, and chocolate éclairs; sandwich fillings; and milk and dairy products.
What is a gram positive bacterium?
What is Staphylococcus aureus? Staphylococcus aur eus is a gram positive bacterium that usually appears under the microscope as spherical (coccus) organisms appearing in pairs, short chains, or bunched, grape-like clusters.
Why is S. aureus a common cause of IE?
aureus is now the most common cause of IE in the industrialized world ( 125 ). Due to its propensity to cause severe disease and its frequent antibiotic resistance, S. aureus is a dreaded cause of IE. Although our ability to rigorously study IE was previously limited by its relative infrequency at any single institution, large multinational collaborations such as the International Collaboration on Endocarditis Prospective Cohort Study (ICE-PCS) ( 126) and robust population-level studies ( 127, – 129) have provided critical insights into the epidemiology and prognosis of IE in general and S. aureus IE in particular.
How much of the human population is contaminated with S. aureus?
Approximately 30% of the human population is colonized with S. aureus ( 1 ). Simultaneously, it is a leading cause of bacteremia and infective endocarditis (IE) as well as osteoarticular, skin and soft tissue, pleuropulmonary, and device-related infections.
What is the primary defense against S. aureus?
The primary defense against S. aureus infection is the neutrophil response. When S. aureus enters the skin, neutrophils and macrophages migrate to the site of infection. S. aureus evades this response in a multitude of ways, including blocking chemotaxis of leukocytes, sequestering host antibodies, hiding from detection via polysaccharide capsule or biofilm formation, and resisting destruction after ingestion by phagocytes.
How common are osteoarticular infections in children?
The incidence of osteoarticular infections in children ranges from 7 to 22 per 100,000 person-years based on studies from Europe ( 493, – 495 ). These infections are more common in males than in females (with incidences in French children of 24 per 100,000 person-years for boys and 19 per 100,000 person-years for girls) and in toddlers than in other age groups ( 494, 495 ). Some ethnic groups may be at higher risk, with Maori and Pacific Islander populations being overrepresented in a study involving 813 cases of acute OM in New Zealand ( 496 ). In the United States, CA-MRSA has become considerably more prominent as a cause of acute osteoarticular infections since 2000. In a study of 158 cases in Tennessee, the proportion of osteoarticular infections due to CA-MRSA rose from 4% to 40% from 2000 to 2004 ( 497 ). Similarly, the proportion of cases of acute OM due to CA-MRSA was 6% in 1999 to 2001 compared to 31% in 2001 to 2003 in Dallas, TX ( 498 ). In Houston, TX, between 2001 and 2010, 195 of 376 (52%) cases of S. aureus OM were due to MRSA ( 499 ).
What is the most common pathogen in osteoarticular infections?
S. aureus is the most common pathogen in all three major classes of osteoarticular infection, namely, osteomyelitis (OM) ( 382, – 392 ), native joint septic arthritis ( 393, – 401 ), and prosthetic joint infection (PJI) ( 402, – 406 ). As staphylococcal osteoarticular infections in children are common and have distinctive clinical and management issues compared to those in adults, we include an in-depth discussion of this important subpopulation.
How long should I take antibiotics for SAB?
The recommended duration of intravenous (i.v.) antibiotics for uncomplicated SAB is at least 2 weeks. In a recent prospective cohort study of uncomplicated SAB (as defined by IDSA criteria), receipt of antibiotic therapy for <2 weeks was associated with a relapse rate of 8% (compared to 0% for those treated for at least 2 weeks) ( 99 ). This relapse rate is consistent with the 6% rate of late complications (inclusive of relapse and metastatic complications) for intravascular catheter-associated SAB treated for <2 weeks identified in a 1993 meta-analysis of 11 studies ( 100 ). Although a few observational studies have suggested that as little as 7 days of i.v. antibiotics may be adequate (reviewed by Thwaites et al. [ 77 ]), such abbreviated courses must be regarded as investigational pending robust, generalizable evidence. Until such evidence exists, all patients with uncomplicated SAB should receive at least 2 weeks of i.v. antibiotics ( 73, 78, 79 ). Two-week courses of therapy, both with ( 101, – 104) and without ( 102) adjunctive aminoglycosides, have also been used successfully for uncomplicated, IDU-associated, right-sided S. aureus IE. Cure rates in these studies ranged from 77 to 94% ( 101, – 103, 105) and were similar for those who did and those who did not receive adjunctive aminoglycosides. However, cure rates were lower for patients who received glycopeptides (e.g., vancomycin and teicoplanin) than for those receiving antistaphylococcal penicillins ( 101, 105 ). Thus, patients being treated with vancomycin for right-sided IE should receive >2 weeks of therapy. For complicated SAB, 4 to 6 weeks of i.v. therapy has been the standard practice for over half a century and continues to be recommended ( 73, 75, 79, 106 ).
What causes a nidus to form?
The formation of a nidus for bacterial colonization and infection begins with damage to the cardiac endothelium, either by direct trauma (e.g., intravascular catheters and electrodes, injected particulate matter from injection drug use, or turbulent blood flow resulting from valvular abnormalities) or inflammation (e.g., secondary to rheumatic heart disease or degenerative valvular disease). The exposure of subendothelial cells elicits the production of extracellular matrix proteins and tissue factor and the deposition of fibrin and platelets to form sterile vegetations. If these thrombotic vegetations become colonized by bacteria, IE can result ( 155 ).
What is the most common cause of S. aureus infection?
Staphylococcus aureus is a virulent pathogen that is currently the most common cause of infections in hospitalized patients. S. aureus infection can involve any organ system. The success of S. aureus as a pathogen and its ability to cause such a wide range of infections are the result of its extensive virulence factors. The increase in the resistance of this virulent pathogen to antibacterial agents, coupled with its increasing prevalence as a nosocomial pathogen, is of major concern. The core resistance phenotype that seems to be most associated with the persistence of S. aureus in the hospital is methicillin resistance. Methicillin resistance in nosocomial S. aureus isolates has been increasing dramatically in United States hospitals and is also associated with resistance to other useful antistaphylococcal compounds. Possible ways to decrease the incidence of nosocomial S. aureus infections include instituting more effective infection control, decreasing nasal colonization, developing vaccines, and developing new or improved antimicrobials.
How to reduce the incidence of S. aureus?
aureus infections include instituting more effective infection control, decreasing nasal colonization, developing vaccines, and developing new or improved antimicrobials.
