
What is peritoneum and its function?
The peritoneum is the serous membrane that lines the abdominal cavity. It is composed of mesothelial cells that are supported by a thin layer of fibrous tissue and is embryologically derived from the mesoderm. The peritoneum serves to support the organs of the abdomen and acts as a conduit for the passage of nerves, blood vessels, and lymphatics.
What part of the peritoneum covers the stomach?
What is Peritoneum
- Parietal Peritoneum. The parietal peritoneum is the part of the peritoneum lining the internal surface of the abdominopelvic wall.
- Visceral Peritoneum. Visceral peritoneum is the second part of the peritoneum, covering the outer layer of most of the abdominal viscera.
- Peritoneal Cavity. ...
What does peritoneal cavity mean?
The peritoneal cavity is a potential space found between the parietal and visceral layers of the peritoneum. The cavity is filled with a small amount of serous peritoneal fluid secreted by the mesothelial cells which line the peritoneum.
Where are the ovaries, fallopian tubes and peritoneum?
The ovaries and fallopian tubes are parts of the female reproductive system. They are supported by a layer of tissue called the peritoneum. The ovaries are two small, oval-shaped organs in the pelvis. The pelvis is the area between the hips in the lower part of the tummy. The ovaries are part of the female reproductive system.

What is the peritoneum and what is its function?
The peritoneum serves to support the organs of the abdomen and acts as a conduit for the passage of nerves, blood vessels, and lymphatics. Although the peritoneum is thin, it is made of 2 layers with a potential space between them.
Is the peritoneal cavity the same as abdominal cavity?
So let's start with the basics; the Peritoneum is a serous membrane which lines the walls of the abdominal cavity and lies on abdominal and pelvic organs. Between its two layers – parietal and visceral – is the peritoneal cavity. The peritoneum functions to support and protect abdominopelvic organs.
Are kidneys in peritoneal cavity?
The location of the kidneys That is, they are located behind the smooth peritoneal lining of the upper part of the abdominal cavity, between it and the posterior body wall. Therefore, they are actually outside the peritoneal cavity. The kidneys are situated below the diaphragm, one on either side of the spine.
What is the peritoneum of the abdominal cavity?
Your peritoneum is the tissue that lines your abdominal wall and covers most of the organs in your abdomen. A liquid, peritoneal fluid, lubricates the surface of this tissue. Disorders of the peritoneum are not common.
What 2 organs are most visible in the peritoneal cavity?
The cavity is dominated by the liver (large, brown organ at anterior of cavity) and the small intestine, but the large intestine may be visible. The abdominal wall to the left and right of the midline incisions and the umbilical region have been "reflected" (pulled aside to show beneath).
What organ is in the peritoneal cavity?
The space within the abdomen that contains the intestines, the stomach, and the liver. It is bound by thin membranes.
Does the peritoneum grow back?
When traumatized, whether by surgery or due to inflammatory processes, a series of responses come into action to regenerate the injured part of the peritoneum.
Which organs are not covered by peritoneum?
The peritoneum is a closed cavity that contains all of the abdominal organs except for the kidneys and the adrenal glands. The parietal peritoneum covers the abdominal wall and diaphragm.
How does peritoneum heal?
(C) Healing of the peritoneum occurs primarily by re-epithelialization of the damaged site. New mesothelial cells are attracted to the site of injury by chemotactic messengers released by platelets, blood clots, or leukocytes within the injured tissue. At this point, healing of the peritoneum differs from that of skin.
Can the peritoneum be removed?
If surgery is possible, the operation is called a peritonectomy. This means removing part or all of the lining of the abdomen (peritoneum). The aim is to reduce symptoms.
What is the other name for peritoneum?
What is another word for peritoneum?membranefilmtissuelayerskinamnioncauldiaphragmintegumentmucosa2 more rows
What are the three types of peritoneum?
The parietal peritoneum covers the inside of the abdominal wall. The visceral peritoneum covers the intraperitoneal organs. The double-layered peritoneum forms the mesentery that suspends these organs from the abdominal wall. Posterior Abdominal Wall: Anatomy , which lines the inner abdominal wall.
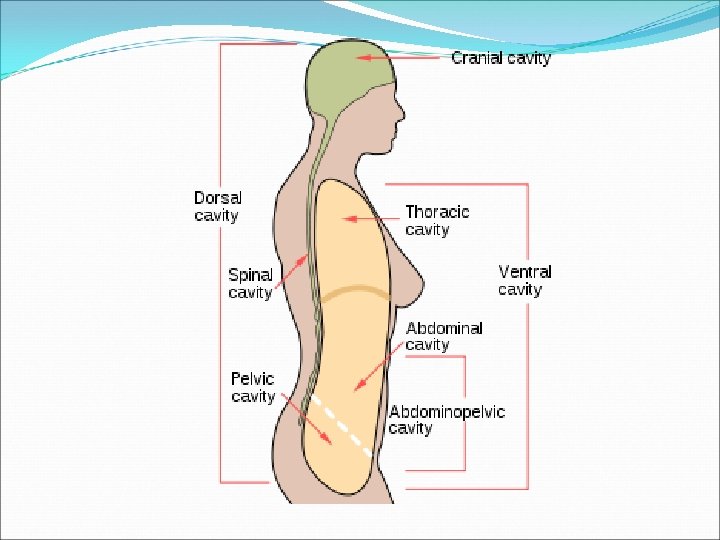
What is the abdominal cavity?
abdominal cavity, largest hollow space of the body. Its upper boundary is the diaphragm, a sheet of muscle and connective tissue that separates it from the chest cavity; its lower boundary is the upper plane of the pelvic cavity. Vertically it is enclosed by the vertebral column and the abdominal and other muscles.
What does peritoneal mean in medical terms?
(PAYR-ih-toh-NEE-ul) Having to do with the parietal peritoneum (the tissue that lines the abdominal wall and pelvic cavity) and visceral peritoneum (the tissue that covers most of the organs in the abdomen, including the intestines).
Where is abdominal cavity located?
The abdominal cavity is a large body cavity in humans and many other animals that contains many organs. It is a part of the abdominopelvic cavity. It is located below the thoracic cavity, and above the pelvic cavity.
Which structure is found in the abdominal cavity?
The abdomen contains many vital organs: the stomach, the small intestine (jejunum and ileum), the large intestine (colon), the liver, the spleen, the gallbladder, the pancreas, the uterus, the fallopian tubes, the ovaries, the kidneys, the ureters, the bladder, and many blood vessels (arteries and veins).
What is contained in the peritoneal cavity?
The peritoneal cavity (abdominal cavity or coelum) houses the visceral organs, which include the liver, stomach, small and large intestines, and ot...
Are the kidneys located in the pelvic cavity?
Terminology used in anatomy The abdominal-pelvic cavity is a bodily cavity formed by the abdominal cavity and the pelvic cavity. The stomach, liver...
What cavity contains the reproductive and excretory system?
The abdominal-pelvic cavity is a bodily cavity formed by the abdominal cavity and the pelvic cavity. It also houses the urine bladder and reproduct...
Where is the peritoneal located?
Stomach cavity. The peritoneal membrane is a thin, transparent membrane that covers the abdominal wall and the organs within the abdomen. It functi...
What is the difference between peritoneal and peritoneum?
The peritoneum is a thin membrane that borders the abdominal and pelvic cavities and covers the majority of the viscera in the abdomen. These cavit...
What organs does the peritoneum cover?
There are two layers to the peritoneum: the superficial parietal layer and the deep visceral layer. The kidneys, urinary bladder, uterus, fallopian...
What is the fold of the peritoneum that suspends organs from the posterior abdominal wall?
The mesentery is the folds of peritoneum that suspend organs from the posterior abdominal wall. Mesentery (diagram) The projection of an organ into the peritoneum creates a peritoneal fold which extends from the abdominal wall, wraps around that organ, and extends back to the abdominal wall.
What is the infracolic compartment?
The infracolic compartment is posterior and inferior to the transverse mesocolon. Looking from the anterior aspect, it is divided by the root of the mesentery of the small intestine into the right and left infracolic spaces. The infracolic compartment contains the small intestine, ascending colon and descending colon.
How do organs push into the peritoneum?
As organs develop and grow, they push into the peritoneum without entering the peritoneal cavity. The cavity squeezes through any available space that exists between the abdominal organs forming peritoneal folds and pouches. It is the same idea as pressing your hand into a balloon filled with water; the balloon changes shape around your hand but your hand doesn’t go inside the balloon. Likewise, no organs lie within this potential space.
What causes ascites in the peritoneum?
The most common cause is increased pressure in the hepatic portal vein, portal hypertension. Portal hypertension is most often seen in people with liver cirrhosis. Ascites clinically presents as a bulging belly showing waves of moving fluid when gently struck – this is not the case for fat tissue.
What are the two layers of the peritoneum?
The peritoneum consists of two layers: 1 Parietal peritoneum – an outer layer which adheres to the anterior and posterior abdominal walls. 2 Visceral peritoneum – an inner layer which lines the abdominal organs. It's made when parietal peritoneum reflects from the abdominal wall to the viscera.
What is the peritoneum?
So let’s start with the basics; the Peritoneum is a serous membrane which lines the walls of the abdominal cavity and lies on abdominal and pelvic organs. Between its two layers – parietal and visceral – is the peritoneal cavity.
What are the two divisions of the peritoneal cavity?
There are two divisions of the peritoneal cavity: lesser sac (omental bursa) and greater sac.
How does intraperitoneal fluid flow?
The natural flow of intraperitoneal fluid occurs along pathways determined by the anatomic compartmentalization of the peritoneal cavity, intraperitoneal pressure, position of the patient , site of fluid origin, nature of fluid, speed of fluid accumulation, presence of adhesions or previous surgery, degree of bladder distention , and density of fluid ( Fig. 111-3 ). 5,6,54–58 Abscesses form and malignant cells grow where natural flow allows the affected ascitic fluid to pool. Fluid in the inframesocolic space seeks the pelvis but may first seed the superior aspect of the sigmoid colon on the left and the medial aspect of the cecum on the right. In the pelvis, infected and malignant fluid fills the pouch of Douglas and then the lateral paravesical recesses. Pelvic fluid then ascends both paracolic gutters, driven by negative intraabdominal pressure associated with respiration, volume considerations, and the topographic anatomy of peritoneal recesses. 5,54 The flow in the left paracolic gutter is modest and limited by the phrenicocolic ligament. Most flow occurs in the right paracolic space. Fluid in this gutter has access to the Morison pouch, the right subphrenic space, and potentially, the lesser sac through the anterior subhepatic space and foramen of Winslow. The falciform ligament usually prevents fluid spread across the midline from the right to the left subphrenic spaces. 51–58
How many intraperitoneal spaces are there in the abdomen?
The peritoneal cavity can be divided into supramesocolic and inframesocolic spaces by the transverse mesocolon. Four intraperitoneal spaces are present in the supramesocolic portion of the abdomen: the suprahepatic and subhepatic spaces on the right and the subphrenic space and lesser sac on the left.
How are paracolic gutters formed?
The paracolic gutters are formed by reflections of peritoneum covering the ascending and descending colon and the lateral abdominal wall. Note the innumerable potential peritoneal recesses lying between the bowel loops and their mesenteric leaves.
What are the folds of the peritoneum?
All double-layered folds of peritoneum, other than mesentery and omentum, are peritoneal ligaments. •. Connect 1 viscus to another (e.g., splenorenal ligament) or viscus to abdominal wall (e.g., falciform ligament) •. Contain blood vessels or remnants of fetal vessels.
What is the left supramesocolic space?
Left supramesocolic space: Divided into left perihepatic spaces (anterior and posterior) and left subphrenic (anterior perigastric and posterior perisplenic)
What is the eponym of Morison?
Many have eponyms [e.g., Morison pouch for posterior subhepatic (hepatorenal) recess; pouch of Douglas for rec touterine recess]
Which compartments are in Winslow's foramen?
Compartments include right and left supramesocolic and inframesocolic spaces, paracolic gutters and pelvic cavity. The peritoneal cavity normally contains a small amount of lubricating fluid.
What is the space between the parietal peritoneum and the visceral peritoneum?
Peritoneal cavity. The peritoneal cavity is a potential space between the parietal peritoneum (the peritoneum that surrounds the abdominal wall) and visceral peritoneum (the peritoneum that surrounds the internal organs).
What is the parietal peritoneum?
The parietal and visceral peritonea are layers of the peritoneum named depending on their function/location. It is one of the spaces derived from the coelomic cavity of the embryo, the others being the pleural cavities around the lungs and the pericardial cavity around the heart.
What is the peritoneal cavity?
The peritoneal cavity is a common injection site, used in intraperitoneal injection . An increase in the capillary pressure in the abdominal viscera can cause fluid to leave the interstitial space and enter the peritoneal cavity, a condition called ascites .
How much fluid does the serosal sac secrete?
It is the largest serosal sac, and the largest fluid-filled cavity, in the body and secretes approximately 50 ml of fluid per day. This fluid acts as a lubricant and has anti-inflammatory properties.
How is cerebrospinal fluid diverted?
In cases where cerebrospinal fluid builds up, such as in hydrocephalus, the fluid is commonly diverted to the peritoneal cavity by use of a shunt placed by surgery.
Which cavity is involved in peritoneal dialysis?
The peritoneal cavity is involved in peritoneal dialysis .
What is the infracolic compartment?
Infracolic compartment – lies below the transverse mesocolon and contains the small intestine, ascending and descending colon. The infracolic compartment is further divided into left and right infracolic spaces by the mesentery of the small intestine.
What is the greater sac?
The greater sac is the larger portion of the peritoneal cavity. It is further divided into two compartments by the mesentery of the transverse colon (known as the transverse mesocolon): Supracolic compartment – lies above the transverse mesocolon and contains the stomach, liver and spleen.
What is the difference between a greater and lesser peritoneal sac?
The peritoneal cavity can be divided into the greater and lesser peritoneal sacs. The greater sac comprises the majority of the peritoneal cavity. The lesser sac (also known as the omental bursa) is smaller and lies posterior to the stomach and lesser omentum.
Why is the peritoneal cavity referred to as a potential space?
While the peritoneal cavity is ordinarily filled with only a thin film of fluid, it is referred to as a potential space because excess fluid can accumulate in it, resulting in the clinical condition of ascites (see clinical applications).
Why is the peritoneal cavity different from the pelvic cavity?
Due to the presence of different pelvic organs, the peritoneal cavity differs in structure between the sexes. The primary difference in structure is the location of the most distal portion of the cavity.
Which compartments are connected by paracolic gutters?
The supracolic and infracolic compartments are connected by the paracolic gutters which lie between the posterolateral abdominal wall and the lateral aspect of the ascending or descending colon.
Which is larger, the peritoneal cavity or the greater sac?
The greater sac comprises the majority of the peritoneal cavity. The lesser sac (also known as the omental bursa) is smaller and lies posterior to the stomach and lesser omentum. Greater Sac. The greater sac is the larger portion of the peritoneal cavity.
What are the two layers of the peritoneum?
The peritoneum consists of two layers that are continuous with each other: the parietal peritoneum and the visceral peritoneum. Both types are made up of simple squamous epithelial cells called mesothelium.
How are the abdominal viscera divided?
The abdominal viscera can be divided anatomically by their relationship to the peritoneum. There are two main groups: intraperitoneal and retroperitoneal organs.
What is the visceral peritoneum?
The visceral peritoneum invaginates to cover the majority of the abdominal viscera. It is derived from splanchnic mesoderm in the embryo.
Where does the parietal peritoneum originate?
The parietal peritoneum lines the internal surface of the abdominopelvic wall. It is derived from somatic mesoderm in the embryo. It receives the same somatic nerve supply as the region of the abdominal wall that it lines; therefore, pain from the parietal peritoneum is well localised.
Where is the omenta located?
The omenta are sheets of visceral peritoneum that extend from the stomach and proximal part of the duodenum to other abdominal organs.
Which part of the body covers the viscera?
The peritoneum covers nearly all viscera within the gut and conveys neurovascular structures from the body wall to intraperitoneal viscera.
Why is the abdominal policeman called the policeman?
It has a role in immunity and is sometimes referred to as the ‘ abdominal policeman ’ because it can migrate to infected viscera or to the site of surgical disturbance.
How much serous fluid is in the peritoneal cavity?
Normally, the peritoneal space only contains up to 100 mL of serous fluid. In various situations, such as cirrhosis or chyle leaks, there can be a pathologic increase in peritoneal fluid volume. Cirrhotic ascites is believed to be due to portal hypertension, leading to increased permeability in blood vessels, allowing for altered oncotic and hydrostatic pressures that result in an imbalance of protein and electrolytes, thus altering the fluid flow.[13] In chylous ascites, there is an increase in lymphatic fluid in the peritoneal cavity, which can be secondary to a chyle leak or can occur from surgery or trauma.[14] Treatment is primarily medical but can be surgical on occasion.
What are the two layers of the peritoneum?
The peritoneum is comprised of 2 layers: the superficial parietal layer and the deep visceral layer. The peritoneal cavity contains the omentum, ligaments, and mesentery. Intraperitoneal organs include the stomach, spleen, liver, first and fourth parts of the duodenum, jejunum, ileum, transverse, and sigmoid colon. Retroperitoneal organs lie behind the posterior sheath of the peritoneum and include the aorta, esophagus, second and third parts of the duodenum, ascending and descending colon, pancreas, kidneys, ureters, and adrenal glands.
What is the epiploic foramen?
An important space in the peritoneal cavity is the epiploic foramen, also known as the foramen of Winslow. This foramen allows communication between the greater and lesser sacs. It is bordered by the hepatoduodenal ligament anteriorly, the inferior vena cava (IVC) posteriorly, duodenum inferiorly, and the caudate lobe of the liver superiorly. The foramen provides access to a surgeon, should they need to clamp the hepatoduodenal ligament to stop a hemorrhage or gain anatomical access to the lesser sac. The foramen can also serve as a location for a lesser sac hernia.
What is the function of the dorsal mesentery?
It acts as a protective or insulating layer. The mesentery helps attach the abdominal organs to the abdominal wall and contains many blood vessels, nerves, and lymphatics. Intraperitoneal organs are usually mobile while those in the retroperitoneum are usually fixed to the posterior abdominal wall. The dorsal mesentery also gives off the transverse and sigmoid mesocolons, which are important due to them containing the blood, nerve, and lymphatic supply for related structures.
What is the role of the peritoneum in a hernia?
The peritoneum plays a significant role in surgical planning for inguinal hernia repairs. The peritoneum is significant enough that the laparoscopic approaches refer to the relationship to the peritoneum with options of a transabdominal pre-peritoneal (TAPP) or total extra pre-peritoneal (TEPP) repairs. In a TAPP, the peritoneum is penetrated, and the surgeon works to repair a hernia from an iatrogenic hole dissected to access the hernia sac that is then primarily closed. A TEPP avoids the peritoneum altogether by staying superficial to it to access the hernia sac and repair it. [5]
Why is the innervation of the peritoneum important?
A thorough understanding of the innervation of the peritoneum is important as it has clinical implications. The peritoneum has both somatic and autonomic innervations that help explain why various abdominal pathologies, such as peritonitis or appendicitis present the way they do. The parietal peritoneum receives its innervation from spinal nerves T10 through L1. This innervation is somatic and allows for the sensation of pain and temperature that can be localized. The visceral peritoneum receives autonomic innervation from the Vagus nerve and sympathetic innervation that result in the difficult to localize abdominal sensations triggered by organ distension. [2][4]
What is the peritoneum used for?
The peritoneum is also utilized in therapeutic approaches for hydrocephalus. Patients who want definitive treatment for their hydrocephalus or are refractory to medical management can pursue surgical management via a ventriculoperitoneal shunt where the excess cerebrospinal fluid is shunted to the peritoneum, where it is then reabsorbed by the body more appropriately.
What causes peritonitis in peritoneal dialysis?
Often, peritonitis associated with peritoneal dialysis is caused by germs around the tube (catheter). If you're receiving peritoneal dialysis, take the following steps to prevent peritonitis:
Why does peritoneal dialysis cause infection?
An infection may occur during peritoneal dialysis due to unclean surroundings, poor hygiene or contaminated equipment.
What causes bacteria to enter the peritoneum?
Any of these conditions can allow bacteria to get into the peritoneum through a hole in your gastrointestinal tract. Pancreatitis. Inflammation of your pancreas (pancreatitis) complicated by infection may lead to peritonitis if the bacteria spreads outside the pancreas. Diverticulitis.
What is the term for a complication of liver disease?
Peritonitis that develops without an abdominal rupture (spontaneous bacterial peritonitis) is usually a complication of liver disease, such as cirrhosis. Advanced cirrhosis causes a large amount of fluid buildup in your abdominal cavity. That fluid buildup is susceptible to bacterial infection.
Why does my peritoneum smell?
Peritonitis may result from a burst appendix or trauma-related abdominal injury. Seek immediate medical attention if you develop abdominal pain so severe that you're unable to sit still or find a comfortable position.
What causes a pouch to rupture?
Diverticulitis. Infection of small, bulging pouches in your digestive tract (diverticulosis) may cause peritonitis if one of the pouches ruptures, spilling intestinal waste into your abdominal cavity.
What to do if you have abdominal pain after an accident?
Call 911 or seek emergency medical assistance if you have severe abdominal pain following an accident or injury.
Overview
The peritoneal cavity is a potential space between the parietal peritoneum (the peritoneum that surrounds the abdominal wall) and visceral peritoneum (the peritoneum that surrounds the internal organs). The parietal and visceral peritonea are layers of the peritoneum named depending on their function/location. It is one of the spaces derived from the coelomic cavity of the embryo, the others being the pleural cavities around the lungs and the pericardial cavity around th…
Compartments
The peritoneal cavity is divided by the transverse colon (and its mesocolon) into an upper supracolic compartment, and a lower infracolic compartment. The liver, spleen, stomach, and lesser omentum are contained within the supracolic compartment. The small intestine surrounded by the ascending, transverse, and descending colon, and the paracolic gutters are contained within the infracolic compartment.
Clinical significance
The peritoneal cavity is a common injection site, used in intraperitoneal injection.
An increase in the capillary pressure in the abdominal viscera can cause fluid to leave the interstitial space and enter the peritoneal cavity, a condition called ascites.
In cases where cerebrospinal fluid builds up, such as in hydrocephalus, the fluid is commonly diverted to the peritoneal cavity by use of a shunt placed by surgery.
See also
• Lesser sac
• Greater sac
External links
• peritoneum at The Anatomy Lesson by Wesley Norman (Georgetown University)