The juxtaglomerular cells secrete renin in response to:
- Stimulation of the beta-1 adrenergic receptor
- Decrease in renal perfusion pressure (detected directly by the juxtaglomerular cells)
- Decrease in NaCl concentration at the macula densa, often due to a decrease in glomerular filtration rate
What causes juxtaglomerular release of renin?
Mechanism of Action Increased renin release from the juxtaglomerular cells is caused by several conditions: reduction in renal blood flow from heart failure, blood loss, hypotension or ischemia of the kidneys, sodium diuresis (excessive sodium loss in urine), and beta-adrenergic stimulation.
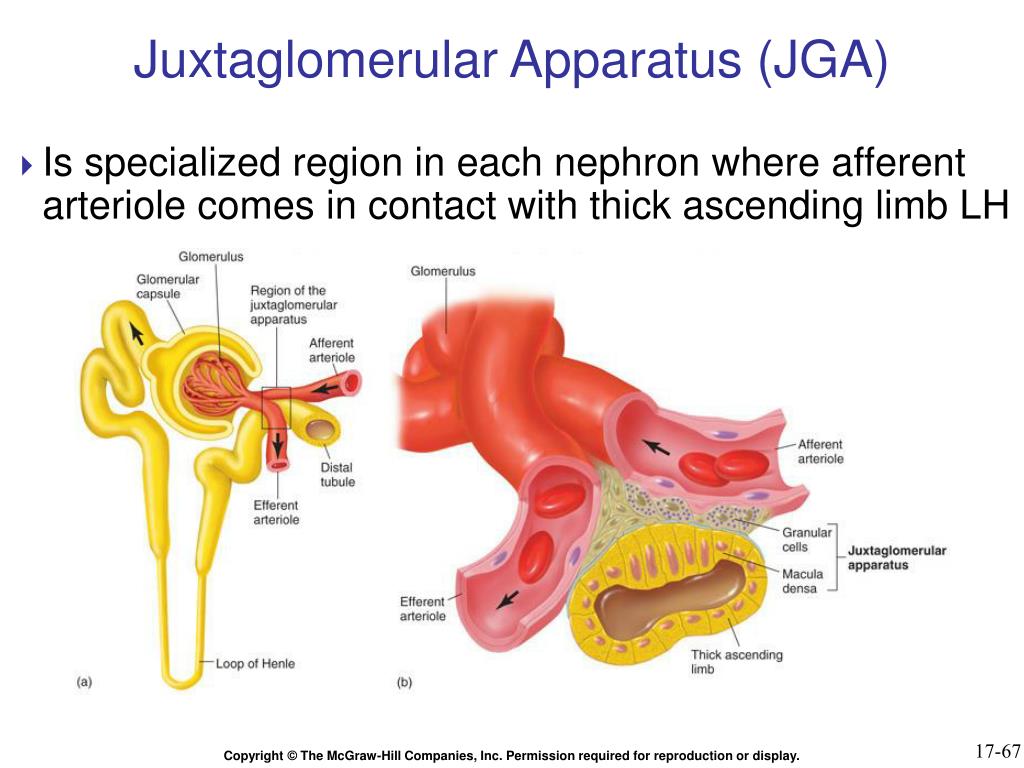
What is the function of juxtaglomerular apparatus?
juxtaglomerular apparatus in the nephron, the complex of cells from the distal tubule and the afferent arteriole which helps regulate blood pressure by secreting renin in response to blood pressure changes in the kidney; located near the glomerulus macula densa cells
What is the function of renin in the nephron?
in the nephron, the complex of cells from the distal tubule and the afferent arteriole which helps regulate blood pressure by secreting renin in response to blood pressure changes in the kidney; located near the glomerulus macula densa cells specialized chemoreceptors
Where is the juxtaglomerular apparatus in the nephron?
juxtaglomerular apparatus in the nephron, the complex of cells from the distal tubule and the afferent arteriole which helps regulate blood pressure by secreting renin in response to blood pressure changes in the kidney; located near the glomerulus macula densa cells specialized chemoreceptors release vasoconstrictors found in DCT
What stimulates the release of renin from the juxtaglomerular apparatus quizlet?
Renin is secreted by the juxtaglomerular cells in response sympathetic stimulation and low blood pressure.
What stimulates the release of renin quizlet?
1. Reduction in blood pressure at afferent arteriole of the kidney stimulates renin release from kidney.
What hormone stimulates renin release?
There is also a potent pressure-sensitive mechanism for renin release; its stimulation is associated with activation of the sympathetic nervous system and release of hormones, such as oxytocin, which stimulate renin release in rats via a β-adrenergic receptor-dependent mechanism (Huang et al.
What causes the release of renin?
Renin is released into your bloodstream when your blood pressure drops too low or when there's not enough sodium in your body. Specifically, renin secretion happens when: Baroreceptors (pressure-sensitive receptors) in your arterial vessels detect low blood pressure. Your kidneys detect low salt (sodium) levels.
Where is renin released from quizlet?
Where is renin secreted from? Juxtaglomerular cells.
What are the 3 stimuli that cause the release of renin?
Its release is stimulated by: sympathetic nerve activation (acting through β1-adrenoceptors) renal artery hypotension (caused by systemic hypotension or renal artery stenosis)
What signals renin release?
Renin secretion and synthesis are essentially triggered by sympathetic nerve activity with noradrenaline as the main stimulatory transmitter acting via β1 receptors on JGE cells.
Does stimulation of JG cells stimulate renin release?
Discussion. Catecholamines and other renin-stimulating hormones stimulate renin release from renal JG cells via G protein–coupled receptors, Gsα-mediated activation of adenylyl cyclases, and an increase in intracellular cAMP.
What are the 3 stimuli that cause the release of renin?
Its release is stimulated by: sympathetic nerve activation (acting through β1-adrenoceptors) renal artery hypotension (caused by systemic hypotension or renal artery stenosis)
When renin is released from the kidney quizlet?
When blood pressure falls (for systolic, to 100 mm Hg or lower), the kidneys release the enzyme renin into the bloodstream.
What are the effects of renin release quizlet?
Stimulates thirst and increased secretion of ADH in the brain, to increase blood pressure and water retention. 3. Increase aldosterone secretion from the adrenal gland, to increase blood pressure, water retention and sodium retention.
What is the effect of renin quizlet?
Cells in the kidneys respond to low blood pressure by releasing an enzyme called renin. Renin causes the kidneys to reabsorb sodium. Sodium reabsorption, in turn, is always accompanied by water retention. This helps to restore blood volume and blood pressure.
What do macula densa cells do when salt content is high?
If the salt content is high, or the volume of fluid is low, the macula densa cells do two things: 1) tell the granular cells to release renin, and 2) dilate the afferent arteriole of the glomerulus ( by secreting a little vasopressive hormone).
How are extraglomerular cells connected?
The two types are connected by gap junctions. The function of the extraglomerular cells is a bit obscure. They contract when they are stimulated by sympathetic nerves. In addition, they are located in between the macula densa and the afferent arteriole, so maybe they help these two structures communicate.
What do the macula densa cells do?
Macula densa cells are specialized cells within the wall of the distal tubule. They sense the salt content and the volume of fluid within the tubule (which is related to the glomerular filtration rate). If the salt content is high, or the volume of fluid is low, the macula densa cells do two things: 1) tell the granular cells to release renin, ...
What are the different types of cells in the JGA?
There are actually three different types of cells in the JGA: granular cells (which secrete renin), macula densa cells (which secrete a vasopressive substance that acts on the afferent glomerular arteriole) and mesangial cells (whose function is a little obscure).
What are granular cells?
Granular cells (also called juxtaglomerular cells) are little connective tissue cells surrounding glomerular arterioles. They secrete renin in response to three things: 1) beta-adrenergic stimulation, 2) decreased renal perfusion pressure (which is detected by the granular cells themselves) and 3) signals from the macula densa.
Which muscle cells act as mechanoreceptors?
smooth muscle cells that act as mechanoreceptors (stretch receptors)
Which organ is responsible for regulating blood pressure?
in the nephron, the complex of cells from the distal tubule and the afferent arteriole which helps regulate blood pressure by secreting renin in response to blood pressure changes in the kidney; located near the glomerulus
Does afferent arterioles increase GFR?
leads to afferent arterio les dilated and increase in GFR
Which cells regulate renin secretion?
Regulation of renin secretion by renal juxtaglomerular cells
What is the main rate limiting step in the renin-angiotensin-aldoster?
A major rate-limiting step in the renin-angiotensin-aldosterone system is the release of active renin from endocrine cells (juxtaglomerular (JG) cells) in the media layer of the afferent glomerular arterioles. The number and distribution of JG cells vary with age and the physiological level of stimulation; fetal life and chronic stimulation by extracellular volume contraction is associated with recruitment of renin-producing cells. Upon stimulation of renin release, labeled renin granules "disappear;" the number of granules decrease; cell membrane surface area increases in single cells, and release is quantal. Together, this indicates exocytosis as the predominant mode of release. JG cells release few percent of total renin content by physiological stimulation, and recruitment of renin cells is preferred to recruitment of granules during prolonged stimulation. Several endocrine and paracrine agonists, neurotransmitters, and cell swelling converge on the stimulatory cyclic AMP (cAMP) pathway. Renin secretion is attenuated in mice deficient in beta-adrenoceptors, prostaglandin E(2)-EP4 receptors, Gsα protein, and adenylyl cyclases 5 and 6. Phosphodiesterases (PDE) 3 and 4 degrade cAMP in JG cells, and PDE3 is inhibited by cyclic GMP (cGMP) and couples the cGMP pathway to the cAMP pathway. Cyclic AMP enhances K(+)-current in JG cells and is permissive for secretion by stabilizing membrane potential far from threshold that activates L-type voltage-gated calcium channels. Intracellular calcium paradoxically inhibits renin secretion likely through attenuated formation and enhanced degradation of cAMP; by activation of chloride currents and interaction with calcineurin. Connexin 40 is necessary for localization of JG cells in the vascular wall and for pressure- and macula densa-dependent suppression of renin release.
Which hormones stimulate renin secretion?
It has been known for a long time that renin synthesis and secretion are stimulated by the sympathetic nerves and the prostaglandins and are inhibited in negative feedback loops by angiotensin II, high blood pressure, salt, and volume overload.
What is the role of aspartyl protease in the release of renin?
Renin release. The aspartyl-protease renin is the key regulator of the renin-angiotensin-aldosterone system, which is critically involved in salt, volume, and blood pressure homeostasis of the body. Renin is mainly produced and released into circulation by the so-called juxtaglomerular epithelioid cells, located i ….
Where is renin released?
Renin is mainly produced and released into circulation by the so-called juxtaglomerular epithelioid cells, located in the walls of renal afferent arterioles at the entrance of the glomerular capillary network.
Which hormone is the key regulator of the renin-angiotensin-aldosterone system?
The aspartyl-protease renin is the key regulator of the renin-angiotensin-aldosterone system, which is critically involved in salt, volume, and blood pressure homeostasis of the body.
How does the juxtaglomerular apparatus control the glomerular tubular balance?
The key to the control by the juxtaglomerular apparatus of glomerular tubular balance (balancing of GFR and the reabsorption of water and sodium by the tubules) and of blood pressure lies in the inverse relationship between GFR and distal tubule sodium content. If GFR rises due to an increase in blood pressure, then the time available for sodium reabsorption by the tubules falls and the sodium concentration in the distal tubule increases. This stimulates the macula densa cells and leads to the release of adenosine, leading the glomerular vessels to constrict and reducing the GRF. It may be that this constriction of glomerular vessels is mediated by the glomerular mesangial cells, which are known to be contractile.
Which cells secrete renin?
Juxtaglomerular apparatus cells secrete renin into the renal interstitium, thus providing a stimulus for the local generation of Ang I, and this secreted active form contains 339–343 amino acid residues after proteolytic removal of the 43 amino acid residue at the N-terminus of prorenin.
What is the macula densa cell base?
With electron microscopy, the macula densa cell base is seen to interdigitate with the adjacent lacis cells to form a complex relationship. View chapter Purchase book. Read full chapter.
What is the juxtaglomerular apparatus?
The juxtaglomerular apparatus consists of the juxtaglomerular cells of the afferent glomerular arteriole, the efferent glomerular arteriole, the extraglomerular mesangial cells, and that small portion of the distal tubule known as the macula densa that is located beside the renal glomerulus.
Where is the JGA located?
The JGA is located at the vascular pole of the glomerulus, where a portion of the distal nephron comes into contact with its parent glomerulus. The main components of the JGA are the macula densa of the thick ascending limb, the renin-producing granular cells of the afferent arteriole, and the extraglomerular mesangial cell (Goormaghtigh cell, lacis cell; Figure 47.3 ). The macula densa is a specialized region of the TAL adjacent to the hilum of the glomerulus. The cells of macula densa are low columnar and exhibit an apically placed nucleus. With electron microscopy, the macula densa cell base is seen to interdigitate with the adjacent lacis cells to form a complex relationship.
What is the urethra?
The urethra extends from the bladder to the surface of the body. It consists of an epithelium-lined lumen and a smooth muscle layer. Urine exiting the urethra must pass through the muscular external sphincter.
Does ACE inhibition affect renin?
Renin producing cells have a unique origin that allows their abundance along the afferent arteriole to be regulated by various stimuli. ACE inhibition induces a recruitment of cells in afferent arterioles beyond the JGA even though they were not expressing the renin gene in the basal state. 31 Positive renin immunoreactivity has also been observed in the cells of glomeruli and in proximal and distal tubular segments. More recently, increased attention has been focused on the presence of renin mRNA and protein expression in distal nephron segments, specifically in the principal cells of connecting tubules and collecting ducts, suggesting local formation and secretion into the distal tubular fluid. Renin synthesis in principal cells of collecting ducts is further increased by chronic infusions of Ang II. 25,26 Rats chronically infused with Ang II for 13 days show a suppression of plasma renin activity but increases in urinary prorenin content and renin excretion. 16 In addition, the urinary renin and prorenin protein levels, examined by Western blot, are augmented about 10-fold in Ang II-infused rats. Concomitant AT1R blockade with candesartan prevents increases in both urinary and tissue renin and in prorenin levels. Although there is marked suppression of plasma renin activity, increased renin synthesis by CD cells and secretion into the luminal fluid lead to increased urinary levels of renin and prorenin. 16