What are the 12 blood clotting factors?
What are the 12 blood clotting factors? Respectively, each one is named, fibrinogen, prothrombin, Christmas factor, Stuart-Prower factor, plasma thromboplastin, and Hageman factor. The extrinsic pathway consists of factors I, II, VII, and X. Factor VII is called stable factor. Which are the clotting factors? The common pathway factors X, V, II, I, and XIII …
What begins the intrinsic pathway of coagulation?
The intrinsic pathway is initiated by the activation of factor XII by certain negatively charged surfaces, including glass. High-molecular-weight kininogen and prekallikrein are two proteins that bleeding and blood clotting - Intrinsic pathway of blood coagulation | Britannica
What helps blood clot faster?
What helps blood clot faster? Ice. Applying ice to a wound will constrict the blood vessels, allowing a clot to form more quickly and stop the bleeding. The best way to do this is to wrap ice in a clean, dry cloth and place it on the wound. ... Organic sulfur compounds help reduce the level of cholesterol in your body and may also help break ...
What produces coagulation factor VIII?
Coagulation factors are produced from hepatocytes, whereas production of coagulation factor VIII (FVIII) from primary tissues and cell species is still controversial. Here, we tried to characterize primary FVIII-producing organ and cell species using genetically engineered mice, in which enhanced green fluorescent protein (EGFP) was expressed ...
Which organ is involved in coagulation?
One of the organs intimately involved in the coagulation process is the liver . The liver is responsible for the formation of factors I, II, V, VII, VIII, IX, X, XI, XIII, and protein C and S. Factor VII is created by the vascular endothelium.
What is the purpose of coagulation pathway?
The purpose is to ultimately stabilize the platelet plug with a fibrin mesh. [1][2][3] Function. The function of the coagulation pathway is to keep hemostasis, which is the blockage of a bleeding or hemorrhage. Primary hemostasis is an aggregation of platelets forming a plug at the damaged site of exposed endothelial cells.
What are the two pathways that lead to hemostasis?
Two paths, intrinsic and extrinsic, originate separately but converge at a specific point, leading to fibrin activation. The purpose is to ultimately stabilize the platelet plug with a fibrin mesh.[1][2][3] The coagulation pathway is a cascade of events that leads to hemostasis. The intricate pathway allows for rapid healing and prevention ...
What are the factors that are involved in hemostasis?
The intrinsic pathway consists of factors I, II, IX, X, XI, and XII. Respectively, each one is named , fibrinogen, prothrombin, Christmas factor, Stuart-Prower factor,plasma thromboplastin, and Hageman factor. The extrinsic pathway consists of factors I, II, VII, and X. Factor VII is called stable factor. The common pathway consists of factors I, II, V, VIII, X. The factors circulate through the bloodstream as zymogens and are activated into serine proteases. These serine proteases act as a catalyst to cleave the next zymogen into more serine proteases and ultimately activate fibrinogen. The following are serine proteases: factors II, VII, IX, X, XI and XII. These are not serine proteases: factors V, VIII, XIII. The intrinsic pathway is activated through exposed endothelial collagen, and the extrinsic pathway is activated through tissue factor released by endothelial cells after external damage.
What is the primary hemostasis?
Primary hemostasis is an aggregation of platelets forming a plug at the damaged site of exposed endothelial cells. Secondary hemostasis includes the two main coagulation pathways, intrinsic and extrinsic, that meet up at a point to form the common pathway. The common pathway ultimately activates fibrinogen into fibrin.
What is the pathway of secondary hemostasis?
It begins with the activation of Factor XII (a zymogen, inactivated serine protease) which becomes Factor XIIA (activated serine protease) after exposure to endothelial collagen. Endothelial collagen is only exposed when endothelial damage occurs. Factor XIIA acts as a catalyst to activate factor XI to Factor XIA. Factor XIA then goes on to activate factor IX to factor IXA. Factor IXA goes on to serve as a catalyst for turning factor X into factor Xa. This is known as a cascade. When each factor is activated, it goes on to activate many more factors in the next steps. As you move further down the cascade, the concentration of that factor increases in the blood. For example, the concentration of factor IX is more than that of factor XI. When factor II is activated by either intrinsic or extrinsic pathway, it can reinforce the intrinsic pathway by giving positive feedback to factors V, VII, VIII, XI, XIII. This makes factor XII less critical; patients can actually clot well without factor XII. The intrinsic pathway is clinically measured as the partial thromboplastin time (PTT).
Which factor activates fibrinogen?
Factor IIa (thrombin) goes on to activate fibrinogen into fibrin. Thrombin also goes on to activate other factors in the intrinsic pathway (factor XI) as well as cofactors V and VIII and factor XIII. Fibrin subunits come together to form fibrin strands, and factor XIII acts on fibrin strands to form a fibrin mesh.
What is the process of coagulation?
In simple words Coagulation means Clotting which is seen when there is any injury to the body, the Liquid blood turns in gel form which is used to stop the bleeding from the injury site. The Clotting factors are Plasma proteins which are circulating in the Blood stream, they end up being a clot through Enzymatic cascade.
Why is it important to know about blood coagulation?
Knowing about the Blood Coagulation factors in Dentistry is very important to prevent the mishaps from occurring during or after Dental procedures. There are many Hematologic disorders which are related to these factors, which makes it essential to make note of these factors and the concerning disorders.
What are the natural proteins that help in coagulation?
Blood Coagulation or Clotting Factors are the natural proteins which help in coagulation of blood to control bleeding, they also help to maintain the flow of blood in the body and also make sure coagulation takes place in case of any injury.
What is the role of thrombin in clotting?
Most have their own role to play in Clotting, but some Factors play a major role – Thrombin (Factor II) which is a major coagulant as it converts Fibrinogen into Fibrin which forms a major chunk of the Clot in addition to the Platelets.
What factor does Accelerin not exist?
Factor VI – Accelerin (Does not exist as it was named initially but later on discovered not to play a part in blood coagulation)
What are the coagulation factors?
The coagulation factors are generally serine proteases ( enzymes ), which act by cleaving downstream proteins. The exceptions are tissue factor, FV, FVIII, FXIII. Tissue factor, FV and FVIII are glycoproteins, and Factor XIII is a transglutaminase. The coagulation factors circulate as inactive zymogens . The coagulation cascade is therefore classically divided into three pathways. The tissue factor and contact activation pathways both activate the "final common pathway" of factor X, thrombin and fibrin.
When were coagulation factors discovered?
Coagulation factors. The remainder of the biochemical factors in the process of coagulation were largely discovered in the 20th century. A first clue as to the actual complexity of the system of coagulation was the discovery of proaccelerin (initially and later called Factor V) by Paul Owren (1905–1990) in 1947.
What is the term for platelets that form a plug at the site of injury?
Platelets immediately form a plug at the site of injury; this is called primary hemostasis. Secondary hemostasis occurs simultaneously: additional coagulation (clotting) factors beyond factor VII ( listed below) respond in a cascade to form fibrin strands, which strengthen the platelet plug.
How is the coagulation cascade maintained?
The coagulation cascade is maintained in a prothrombotic state by the continued activation of FVIII and FIX to form the tenase complex until it is down-regulated by the anticoagulant pathways.
What are the tests for coagulation?
Numerous tests are used to assess the function of the coagulation system: 1 Common: aPTT, PT (also used to determine INR ), fibrinogen testing (often by the Clauss method ), platelet count, platelet function testing (often by PFA-100 ), thrombodynamics test. 2 Other: TCT, bleeding time, mixing test (whether an abnormality corrects if the patient's plasma is mixed with normal plasma), coagulation factor assays, antiphospholipid antibodies, D-dimer, genetic tests (e.g. factor V Leiden, prothrombin mutation G20210A), dilute Russell's viper venom time (dRVVT), miscellaneous platelet function tests, thromboelastography (TEG or Sonoclot), euglobulin lysis time (ELT).
What is the process of blood clotting?
For other uses, see Coagulation (disambiguation). Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair.
What is the role of tissue factor pathway?
Tissue factor pathway (extrinsic) The main role of the tissue factor pathway is to generate a "thrombin burst", a process by which thrombin, the most important constituent of the coagulation cascade in terms of its feedback activation roles, is released very rapidly.
Where are coagulation factors formed?
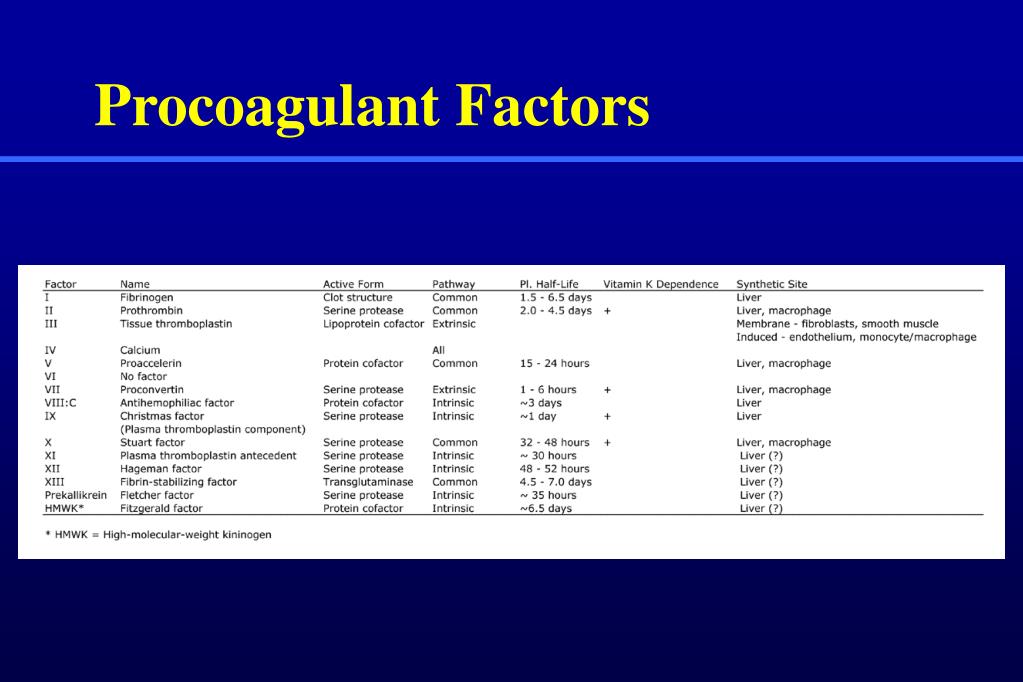
The coagulation factors are formed in the liver. They can be divided into three groups based on their common properties:
What are the factors that affect blood clotting?
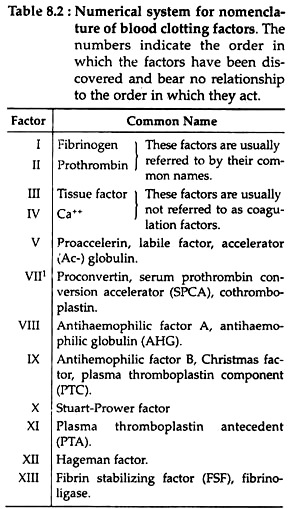
coagulation factors factors essential to normal blood clotting, whose absence, diminution, or excess may lead to abnormality of the clotting. Twelve factors, commonly designated by Roman numerals, have been described (I–V and VII–XIII; VI is no longer considered to have a clotting function). (See table 6.)
What are the components of hemostasis?
Hemostasis involves three components: blood vessel walls, platelets, and plasma coagulation proteins. Primary hemostasis has three major stages involving platelet adhesion, platelet activation, and platelet aggregation. Platelet adhesion is initiated by exposure of the endothelium as a result of damage to blood vessels. Exposed tissue factor–bearing cells trigger the simultaneous binding of von Willebrand factor to exposed collagen and circulating platelets. Activated platelets release a number of procoagulant factors, including thromboxane, a very potent platelet activator, from storage granules. These factors enter the circulation and activate other platelets, and the cycle continues. The activated platelets aggregate at the site of vessel injury, and at this stage of hemostasis, the glycoprotein IIb/IIIa receptors on the activated platelets bind fibrinogen, causing the platelets to stick together and form a plug. There is a balance in health between the prothrombotic or clot formation process and the antithrombotic or clot disintegration process. Simultaneously, the coagulation process or secondary hemostasis occurs. In secondary hemostasis, the coagulation proteins respond to blood vessel injury in an overlapping chain of events. The contact activation (formerly known as the intrinsic pathway) and tissue factor (formerly known as the extrinsic pathway) pathways of secondary hemostasis are a series of reactions involving the substrate protein fibrinogen, the coagulation factors (also known as enzyme precursors or zymogens ), nonenzymatic cofactors (Ca2+ ), and phospholipids. The factors were assigned Roman numerals in the order of their discovery, not their place in the coagulation sequence. Factor VI was originally thought to be a separate clotting factor. It was subsequently proved to be the same as a modified form of factor Va, and therefore, the number is no longer used.
What is the difference between factor I and factor II?
Factor I is a high-molecular-weight plasma protein that is converted to fibrin through the action of thrombin; deficiency conditions are called afibrinogenemia and hypofibrinogenemia. Called also fibrinogen. Factor II is a glycoprotein present in the plasma that is converted into thrombin in the common pathway of coagulation; deficiency is called hypoprothrombinemia. Called also prothrombin. Factor III is involved in the extrinsic pathway of coagulation, activating factor X; called also tissue thromboplastin or factor.
What is factor II in coagulation?
Factor II is a glycoprotein present in the plasma that is converted into thrombin in the common pathway of coagulation; deficiency is called hypoprothrombinemia. Called also prothrombin. Factor III is involved in the extrinsic pathway of coagulation, activating factor X; called also tissue thromboplastin or factor.
What is coagulation in surgery?
coagulation. [ ko-ag″u-la´shun] clotting. 1. in surgery, the disruption of tissue by physical means to form an amorphous residuum, as in electro coagulation or hotocoagulation. 2. in colloid chemistry, solidification of a sol into a gelatinous mass. blood coagulation clotting.
What is the Stuart-Prower factor?
Once activated, it complexes with calcium, phospholipid, and activated factor V to form prothrombinase, which cleaves and activates prothrombin to thrombin. Called also Stuart or Stuart-Prower factor. Factor XI is a stable factor involved in the intrinsic pathway of coagulation, activating factor IX.
What are the three pathways of coagulation?
Coagulation consists of three pathways, the extrinsic, intrinsic, and common path ways, that interact together to form a stable blood clot. The extrinsic and intrinsic coagulation pathways both lead into the final common pathway by independently activating factor X. The extrinsic pathway involves initiation by factor III (i.e., tissue factor) and its interaction with factor VII. Whereas, factors XII, XI, IX, and VIII are utilized in the intrinsic pathway. Then, the common pathway uses factors X, V, II, I, and XIII.
What is the main goal of coagulation?
The main goal of coagulation is to form a stable blood clot to stop bleeding and allow time for the tissue to be repaired.
When is fibrin produced during the coagulation cascade?
Fibrin (factor Ia) is a long, thin protein with branches produced at the end of the coagulation cascade when fibrinogen (factor I) is converted to fibrin, which stabilizes the blood clot.
What are the most important facts to know about the coagulation cascade?
The coagulation cascade refers to the series of steps that occur during the formation of a blood clot after injury by activating a cascade of proteins called clotting factors . There are three pathways: intrinsic, extrinsic, and common. The intrinsic pathway is activated by factors in the blood, while extrinsic is activated by tissue factor. Both pathways result in activation of factor X leading into the common pathway, which ends with converting fibrinogen into fibrin to form a stabilized blood clot. Coagulation disorders occur when there is a deficiency in a clotting factor involved, and the most common disorders are hemophilia and vitamin K deficiency.
What is the common pathway?
The common pathway may result after the activation of factor X at the end of either pathway. The common pathway begins when factor Xa , Va , and calcium bind together , forming a prothrombinase complex. The prothrombinase complex then activates prothrombin (factor II) into thrombin (factor IIa). Next, thrombin cleaves fibrinogen (factor I) into fibrin (factor Ia). Afterwards, thrombin cleaves the stabilizing factor (factor XIII) into XIIIa. Factor XIIIa binds with calcium to then create fibrin crosslinks to stabilize the clot. Thrombin has several functions, including activating platelets (cell fragments involved in clot formation) and activating factors V, VIII, and IX.
What is the coagulation cascade?
The coagulation cascade involves the activation of a series of clotting factors, which are proteins that are involved in blood clotting. Each clotting factor is a serine protease, an enzyme that speeds up the breakdown of another protein. The clotting factors are initially in an inactive form called zymogens. When placed with its glycoprotein co-factor, the clotting factor is activated and is then able to catalyze the next reaction. When a clotting factor becomes activated, it is denoted with an “a” following its respective Roman numeral (e.g. when activated, Factor V becomes Factor Va).
What is the most common bleeding disorder?
Von Willebrand disease is the most common bleeding disorder and is characterized by a deficiency in von Willebrand factor due to an autosomal dominant genetic mutation. The von Willebrand factor is mostly involved in primary hemostasis where it helps platelets stick together. The factor also plays a role in secondary hemostasis by helping stabilize factor VIII.
What is the intrinsic pathway of blood coagulation?
Intrinsic pathway of blood coagulation. All the components necessary for the clotting process to proceed are found in the blood. As such, the proteins required for such clotting to take place are part of the intrinsic pathway of blood coagulation. This pathway involves a series of proteins, protein cofactors, and enzymes, ...
What is the XA factor that binds to thrombin?
Prothrombin binds to the factor Xa–factor V complex and is converted to thrombin, a potent enzyme that cleaves fibrinogen to fibrin, a monomer. The monomer fibrin molecules then link together (polymerize) to form long fibres.
Why is clotting delayed?
Delayed clotting, measured as a prolonged partial thromboplastin time, may be due to a deficiency in the activity of one or more of the blood-clotting factors or to a chemical inhibitor of blood coagulation. Load Next Page.
What is the intrinsic pathway?
The intrinsic pathway is initiated by the activation of factor XII by certain negatively charged surfaces, including glass. High-molecular-weight kininogen and prekallikrein are two proteins that facilitate this activation. The enzyme form of factor XII (factor XIIa) catalyzes the conversion of factor XI to its enzyme form (factor XIa).
What is the function of factor IXA?
Factor IXa assembles on the surface of membranes in complex with factor VIII; the factor IXa–factor VIII complex requires calcium to stabilize certain structures on these proteins associated with their membrane-binding properties. Factor X binds to the factor IXa–factor VIII complex and is activated to factor Xa.
What is the enzyme form of factor XII?
The enzyme form of factor XII (factor XIIa) catalyzes the conversion of factor XI to its enzyme form (factor XIa). Factor XIa catalyzes the conversion of factor IX to the activated form, factor IXa, in a reaction that requires calcium ions.
Why is factor IX blocked?
The process is blocked from further activation because of the lack of calcium ions, which are required for the next reaction, the activation of factor IX . Upon the addition of calcium ions and a phospholipid preparation (which serves as an artificial membrane for the assembly of the blood-clotting protein complexes), ...

Overview
Physiology
When the endothelium is damaged, the normally isolated underlying collagen is exposed to circulating platelets, which bind directly to collagen with collagen-specific glycoprotein Ia/IIa surface receptors. This adhesion is strengthened further by von Willebrand factor (vWF), which is released from the endothelium and from platelets; vWF forms additional links between the platelets' glycoprote…
Assessment
Numerous tests are used to assess the function of the coagulation system:
• Common: aPTT, PT (also used to determine INR), fibrinogen testing (often by the Clauss method), platelet count, platelet function testing (often by PFA-100), thrombodynamics test.
• Other: TCT, bleeding time, mixing test (whether an abnormality corrects if the patient's plasma is mixed with normal plasma), coagulation factor assays, antiphospholipid antibodies, D-dimer, genetic tests (e.g. factor …
Role in disease
Coagulation defects may cause hemorrhage or thrombosis, and occasionally both, depending on the nature of the defect.
Platelet disorders are either congenital or acquired. Examples of congenital platelet disorders are Glanzmann's thrombasthenia, Bernard–Soulier syndrome (abnormal glycoprotein Ib-IX-V complex), gray platelet syndrome (deficient alph…
Pharmacology
The use of adsorbent chemicals, such as zeolites, and other hemostatic agents are also used for sealing severe injuries quickly (such as in traumatic bleeding secondary to gunshot wounds). Thrombin and fibrin glue are used surgically to treat bleeding and to thrombose aneurysms. Hemostatic Powder Spray TC-325 is used to treated gastrointestinal bleeding.
History
Theories on the coagulation of blood have existed since antiquity. Physiologist Johannes Müller (1801–1858) described fibrin, the substance of a thrombus. Its soluble precursor, fibrinogen, was thus named by Rudolf Virchow (1821–1902), and isolated chemically by Prosper Sylvain Denis (1799–1863). Alexander Schmidt suggested that the conversion from fibrinogen to fibrin is the result of an enzymatic process, and labeled the hypothetical enzyme "thrombin" and its precursor "
Other species
All mammals have an extremely closely related blood coagulation process, using a combined cellular and serine protease process. In fact, it is possible for any mammalian coagulation factor to "cleave" its equivalent target in any other mammal. The only non-mammalian animal known to use serine proteases for blood coagulation is the horseshoe crab.
See also
• Agglutination (biology)
• Post-vaccination embolic and thrombotic events