
Central lines terminating in the brachiocephalic trunk or subclavian The subclavian vein is a paired large vein, one on either side of the body, that is responsible for draining blood from the upper extremities, allowing this blood to return to the heart. The left subclavian vein plays a key role in the absorption of fats and lipids, by allowing its products that have been carried by lymph to enter the bloodstream, where it can enter the hepatic portal vein. Their diameter is approxi…Subclavian vein
Where does a central line end up?
A central line (or central venous catheter) is like an intravenous (IV) line. But it is much longer than a regular IV and goes all the way up to a vein near the heart or just inside the heart. A patient can get medicine, fluids, blood, or nutrition through a central line.
Where should the tip of the central line end?
The correct position of the tip of CVC is considered to be in the superior vena cava (SVC) above the level of pericardial reflection. Blood flow conditions are then optimal to keep the catheter away from the intima and to dilute the infused drugs immediately.
What is the end of the central line?
West RuislipThe Central line is a London Underground line that runs through central London, from Epping, Essex, in the north-east to Ealing Broadway and West Ruislip in west London.
Do central lines go in arteries or veins?
A central line is a narrow cannula (flexible plastic tube) inserted into a large vein in the neck, upper chest or groin. It may include up to three separate channels. It can remain in place for a week or more, if necessary.
Where does the end of a PICC line sit?
PICC Lines A PICC line should be within the SVC i.e. angled downward toward the right heart border, but not in the right atrium.
How far should a central line be inserted?
While inserting the CVC in the IJV via the central approach, the depth of insertion could be at 12-13 cm in males and 11-12 cm in females in right-sided catheters, whereas at a depth of 13-14 cm in males and 12-13 cm in females in left-sided ones. At this length the catheter tip could lie in an optimum position.
How long can a central line stay in place?
A central venous catheter can remain for weeks or months, and some patients receive treatment through the line several times a day. Central venous catheters are important in treating many conditions, particularly in intensive care units (ICUs).
Why is the central line so hot?
Why is the Central line so hot? The Central Line is one of the hottest tube lines because of its age and depth beneath the ground. It is one of the oldest lines in London and was opened as The Central Railway in 1900 with early extensions carried out in 1920 and in the 1940s.
Why do they put a central line in neck?
A central line is necessary when you need drugs given through your veins over a long period of time, or when you need kidney dialysis. In these cases, a central line is easier and less painful than having needles put in your veins each time you need therapy.
What vessel does a central line go in?
A central venous catheter is a thin, flexible tube that is inserted into a vein, usually below the right collarbone, and guided (threaded) into a large vein above the right side of the heart called the superior vena cava.
What is the difference between a PICC line and a central line?
A PICC line is a longer catheter that's also placed in the upper arm. Its tip ends in the largest vein of the body, which is why it's considered a central line. PICC stands for "peripherally inserted central-line catheter.” A CVC is identical to a PICC line, except it's placed in the chest or neck.
How do you know if a central line is arterial?
Hold the tube straight up to the ceiling. If the angiocath is in a vein, the column of blood will fall back down to the level of the CVP. If the angiocath is in an artery, the column of blood will continue to rise.
What is the ideal location for the tip of a subclavian central venous catheter?
To minimize the risk of cardiac tamponade, it has been suggested that the tip of the CVC should be located above the cephalic limit of the pericardial reflection, not merely above the junction of the SVC and right atrium (SVC/RA).
How do you verify a central line placement?
Central line placement confirmation has traditionally be done using CXR. Ultrasound provides an easy, accurate, and timely alternative. Use the ultrasound probe to help you locate the vessel, insert your needle, and confirm guidewire placement and catheter tip position.
What is the normal range for central venous pressure?
The central venous pressure can be measured using a central venous catheter advanced via the internal jugular vein and placed in the superior vena cava near the right atrium. A normal central venous pressure reading is between 8 to 12 mmHg. This value is altered by volume status and/or venous compliance.
Can central line be in right atrium?
It is generally agreed that the tip of an inserted central venous catheter (CVC) should not lie within the right atrium. However, the tip of a CVC not inserted to an adequate depth could lie outside the superior vena cava, predisposing to thrombus formation and infection.
What is the angle of a catheter?
This was reduced for left-sided catheters (6/37; 16%). All right-sided catheters lay at an angle <30°. However, 38% (14/37) of left-sided catheters had not crossed the midline, and 59% (22/37) lay at an angle >30° to the vertical. Only 11% (4/37) of left-sided catheters had crossed the midline and lay at an angle of <30°, and all of these lay below the level of the carina. No immediate complications of insertion were identified. See Table 1.
What is the angle of a right sided catheter?
All right-sided catheters lay at an angle <30°. However, 38% (14/37) of left-sided catheters had not crossed the midline, and 59% (22/37) lay at an angle >30° to the vertical. Only 11% (4/37) of left-sided catheters had crossed the midline and lay at an angle of <30°, and all of these lay below the level of the carina.
What is the Creative Commons 4.0 license?
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author (s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Is left sided catheter tip placement better?
There was a wide variation of catheter tip placements accepted without re-positioning. Left-sided catheter tips are more at risk of less precise (and thus potentially nonoptimal) placement. Our results indicate that a clearer placement strategy is required.
What is the ideal placement of the central line tip?
The ideal placement of the central line tip is unknown.
Why is malposition of femoral central venous catheters unheard of?
Malposition of femoral central venous catheters is virtually unheard of. Why? Because we don't check them. If we routinely obtained an X-ray after every femoral cat heter, we would discover that these lines are not always where we intended (for example, one report suggested that 4.5% lie in the lumbar vein; Gocaze 2012 ). Nonetheless, nothing bad seems to happen (although a hemodialysis catheter in the lumbar vein won't work). Overall this supports the concept that the exact location of central lines may not matter.
Why is it important to place a catheter in the right atrium?
A review concluded that the risk of cardiac perforation from a catheter in the right atrium is currently an “urban legend” ( Pittiruti 2015 ). Hemodialysis catheters achieve better flow rates in the right atrium , so some nephrology guidelines recommend intentional placement in the atrium. Catheter placement within the right atrium does not appear to increase arrhythmia significantly ( Vesely 2003; Torres-Millan 2010 ).
What is the best way to exclusion pneumothorax?
A combination of lung ultrasonography, internal jugular vein ultrasonography, and cardiac ultrasonography with a microbubble injection usually allows immediate exclusion of pneumothorax and proof that the catheter is in a intrathoracic vein.
How much does a chest radiograph cost?
[2] It is estimated that 3 million central lines are placed annually in the United States, with a chest radiograph costing almost $200.
Where are microbubbles in the heart?
within the subclavian vein ; Duran-Gehring 2014 ). This ought to be OK as long as catheter malposition within the internal jugular vein is excluded. An X-ray should be considered however.
Which is faster, ultrasound or ultrasound?
Ultrasonography is faster, allowing immediate use of the catheter in emergent situations.
What is a CVC catheter?
A central venous catheter ( CVC ), also known as a central line, central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access.
How to monitor catheter site?
The catheter site should be monitored visually and with palpation (through dressing) on a regular basis to assess for infection.
What is the scar on the left side of the neck?
A dialysis two-lumen catheter inserted on the person's left side. Scars at the base of the neck indicate the insertion point into the left jugular vein.
How to tell if a central line is infected?
If a central line infection is suspected in a person, blood cultures are taken from both the catheter and a vein elsewhere in the body. If the culture from the central line grows bacteria much earlier (>2 hours) than the other vein site, the line is likely infected. Quantitative blood culture is even more accurate, but this method is not widely available.
How do microbes get into the bloodstream?
Microbes can gain access to the bloodstream via a central catheter a number of ways. Rarely, they are introduced by contaminated infusions. They might also gain access to the lumen of the catheter through break points such as hubs. However, the method by which most organisms gain access is by migrating along the portion of the catheter tracking through subcutaneous tissue until they reach the portion of the catheter in the vein. Additionally, bacteria present in the blood may attach to the surface of the catheter, transforming it into a focus of infection.
What is a central line?
Central lines are used to administer medication or fluids that are unable to be taken by mouth or would harm a smaller peripheral vein, obtain blood tests (specifically the "central venous oxygen saturation"), administer fluid or blood products for large volume resuscitation, and measure central venous pressure. The catheters used are commonly 15–30 cm in length, made of silicone or polyurethane, and have single or multiple lumens for infusion.
Where are catheters placed?
These catheters are commonly placed in veins in the neck ( internal jugular vein ), chest ( subclavian vein or axillary vein ), groin ( femoral vein ), or through veins in the arms (also known as a PICC line, or peripherally inserted central catheters).
What is an implanted port?
An implanted port is similar to a tunneled catheter, but an implanted port is placed entirely under the skin. Medicines are given by a needle placed through the skin into the catheter. An implanted port is not as visible as a tunneled catheter, does not require as much daily care, and does not get in the way of a patient’s regular activities as much as a PICC line or a tunneled catheter might.
Why do we need a central venous catheter?
Central venous catheters may be used for the following reason: To give medicines for treatment of pain, infection, or other medical issues (e.g., cancer or heart problems) To provide fluids for nutrition. To help conduct certain medical tests.
How long does a central line last?
A central venous catheter can remain for weeks or months, and some patients receive treatment through the line several times a day.
Where is a tunneled catheter placed?
A tunneled catheter is surgically placed into a vein in the chest or neck and then passed under the skin. One end of the catheter comes out through the skin so medicines can be given right into the catheter. An implanted port is similar to a tunneled catheter, but an implanted port is placed entirely under the skin.
What is a central vein catheter?
What is a central venous catheter, and why is it used? A central venous catheter, also known as a central line, is a tube that doctors place in a large vein in the neck, chest, groin, or arm to give fluids, blood, or medications or to do medical tests quickly.
What is the flow rate of a 22 gauge catheter?
Although 22-gauge catheters may be able to tolerate flow rates up to 5 ml/sec, the 20-gauge or larger catheter is preferable for flow rates of 3 ml/sec or higher. When a 22-gauge catheter is used, the technologist should adjust the injection rate to < 3.0 cc/sec in adults (2.0 cc/sec. in pediatrics) to suit the smaller bore catheter.
What is the max ml/sec for Arrowgard Blue Plus?
The ARROWgard Blue plus pressure injectable CVC is pressure injectable for CT scanning for up to 10 mL/sec. The center lumen is marked with the max ml/sec on the hub of the catheter. The words “No CT” are marked on the lumen that is not to be used for power injection.
How to administer contrast?
When the proper technique is used, contrast medium can safely be administered intravenously by power injector, at high-flow rates of up to 5 mls/second. A short peripheral IV catheter in the antecubital or forearm area is the preferred route for contrast administration. However other routes may need to be used and each is considered separately below. The follow flowchart will assist in the decision of obtaining proper venous access for contrast administration.
What gauge IV line is used for contrast injection?
A peripheral intravenous line (20 gauge) in the antecubital or forearm area is preferred when power injections are needed in adults. Although 22-gauge catheters may be able to tolerate flow rates up to 5 ml/sec, the 20-gauge or larger catheter is preferable for flow rates of 3 ml/sec or higher. When a 22-gauge catheter is used, the technologist should adjust the injection rate to < 3.0 cc/sec in adults (2.0 cc/sec. in pediatrics) to suit the smaller bore catheter.
What is a smart port?
The Smart Port by AngioDynamics is a subcutaneous indwelling central venous access port that is FDA-approved for power injection of contrast. It has distinctive scalloped edges that can be palpated or seen on a CXR or scout view. Note the “CT” is visible on x-ray image of the newer models of ports as an identifier that this port is power injectable. It is indicated for power injection of contrast media up to 5 mL/sec. and 300 psi pressure limit setting, when used with a Gripper Plus Huber needle. They are MRI conditional at 3 Tesla. This is the most common adult chest port currently placed at UCSF.
What is a BARD power port?
The PowerPort by BARD is a subcutaneous indwelling central venous access port that is FDA-approved for power injection of contrast. It has a distinctive triangular shape that can be palpated (three palpable “bumps” arranged in a triangle) or seen on a CXR or scout view (either an opaque rounded triangle or a triangular outline with the letters “CT” under the triangle). It is indicated for power injection of contrast media up to 5 mL/sec and a 300 psi pressure limit setting, when used with a Gripper Plus Huber needle. There are also dual-lumen PowerPorts by BARD.
What is the maximum flow rate for a pediatric injection?
The maximum flow rate and psi for adult injection is 5 mL/sec at <300 psi, and the maximum flow rate and psi for Pediatric is 2 mL/sec at <300 psi. The injection rate will be dependent on the specific catheter type, size, and specific exam protocol.
Overview
A central venous catheter (CVC), also known as a central line(c-line), central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access. Placement of larger catheters in more centrally located veins is often needed in critically ill patients, or in those requiring prolonged intravenous therapies, for more reliable vascular access. These catheters are commonly placed in veins in the neck (internal jugular vein), chest (subclavia…
Medical uses
The following are the major indications for the use of central venous catheters:
1. Difficult peripheral venous access – central venous catheters may be placed when it is difficult to gain or maintain venous access peripherally (e.g. obesity, scarred veins from prior cannulations, agitated patient).
2. Delivery of certain medications or fluids – medications such as vasopressors (e.g., norepinephrine, vasopressin, phenylephrineetc.)…
The following are the major indications for the use of central venous catheters:
1. Difficult peripheral venous access – central venous catheters may be placed when it is difficult to gain or maintain venous access peripherally (e.g. obesity, scarred veins from prior cannulations, agitated patient).
2. Delivery of certain medications or fluids – medications such as vasopressors (e.g., norepinephrine, vasopressin, phenylephrine etc.), chemotherapeutic agents, or hypertonic sol…
Complications
Central line insertion may cause several complications. The benefit expected from their use should outweigh the risk of those complications.
The incidence of pneumothorax is highest with subclavian vein catheterization due to its anatomic proximity to the apex of the lung. In the case of catheterization of the internal jugular vein, the risk of pneumothorax is minimized by the use of ultrasound guidance. For experienced clinicians, the i…
Insertion
Before insertion, the patient is first assessed by reviewing relevant labs and indication for CVC placement, in order to minimize risks and complications of the procedure. Next, the area of skin over the planned insertion site is cleaned. A local anesthetic is applied if necessary. The location of the vein is identified by landmarks or with the use of a small ultrasound device. A hollow needle is advanced through the skin until blood is aspirated. The color of the blood and the rate of its flo…
Catheter flow
The Hagen–Poiseuille equation describes the properties of flow through a rigid tube. The equation is shown below:
The equation shows that flow rate (Q) through a rigid tube is a function of the inner radius (r), the length of the tube (L), and the viscosity of the fluid (μ). The flow is directly related the fourth power of the inner radius of the tube, and inversely related to the length of the tube and viscosit…
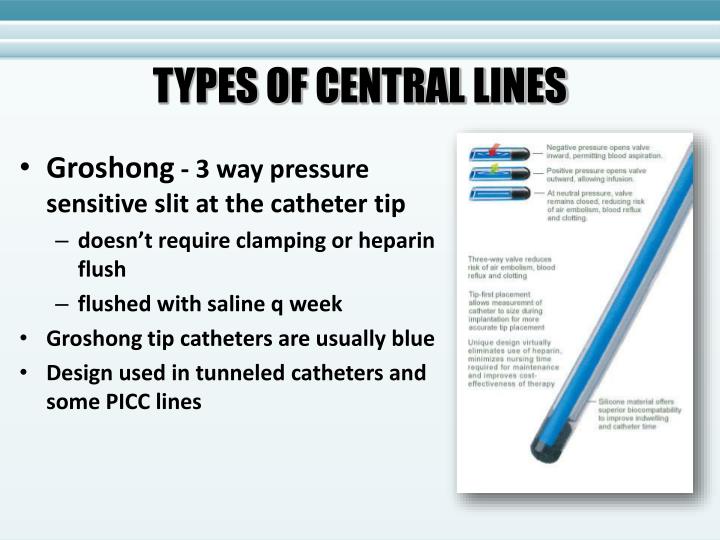
Types
There are several types of central venous catheters; these can be further subdivided by site (where the catheter is inserted into the body) as well as the specific type of catheter used.
A percutaneous central venous catheter, or CVC, is inserted directly through the skin. The internal or external jugular, subclavian, or femoral vein is used. It is most commonly used in critically ill patients. The CVC can be used for days to weeks, and the patient must remain in the hospital. It …
Routine catheter care
The catheter is held in place by an adhesive dressing, suture, or staple which is covered by an occlusive dressing. Regular flushing with saline or a heparin-containing solution keeps the line open and prevents blood clots. There is no evidence that heparin is better than saline at preventing blood clots. Certain lines are impregnated with antibiotics, silver-containing substances (specifically silver sulfadiazine) and/or chlorhexidine to reduce infection risk.
See also
• Peter Pronovost
• Quinton catheter