How long is VRE contagious?
VRE is spread from person to person or by touching a surface touched by someone with VRE. The VRE germ can survive on hard surfaces for five to seven days and on hands for hours. It is easy to stop the spread of VRE with good cleaning and by washing your hands. The germ does not travel through air. How long does it take for VRE to show up?
What is the strongest antibiotic for bacterial infection?
What are the Best Antibiotics for Sinus Infection do Doctors Prescribe For You?
- Amoxicillin – This drug is commonly used to treat acute and uncomplicated bacterial sinusitis. ...
- Cefaclor – This drug is usually used to stop the growth of bacteria and is administered orally. ...
- Sulfamethoxazole – This is an antibacterial medication used to treat infections that occur more frequently on people with a weakened immune system. ...
What are the signs and symptoms of VRE?
- fever,
- chills,
- body aches,
- rapid pulse and breathing,
- nausea and vomiting,
- diarrhea, or
- decreased urination.
What is the treatment for VRE?
When VRE infections do develop, they are generally treated with antibiotics other than vancomycin. In order to identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ.

What is the best antibiotic for VRE?
Tigecycline, a glycylcycline antibiotic, can be used for patients who are intolerant to other agents. It also can be used if other infections are present with the vancomycin-resistant Enterococcus as it has good coverage against gram positives, some gram negatives, and anaerobes.
What is the drug of choice for VRE?
Two novel antimicrobial agents (quinupristin/ dalfopristin and linezolid) have emerged as approved therapeutic options for vancomycin-resistant Enterococcus faecium on the basis of in vitro susceptibility and clinical efficacy from multicentre, pharmaceutical company-sponsored clinical trials.
Which is the drug of choice for VRE and MRSA?
Tigecycline is active against various drug-resistant pathogens, including MRSA, VRE, and many extended β-lactamase, gram-negative bacteria. Tigecycline has a large volume of distribution and produces high concentrations in tissue.
What is VRE and how is it treated?
Enterococci are bacteria (germs) that commonly live in the gastrointestinal tract (bowels) of most people (this is called colonisation) without causing illness. Vancomycin is an antibiotic used to treat infections caused by enterococci.
How is VRE infection treated?
VRE infections may be difficult to cure because the bacteria do not respond to many antibiotics. If you have an infection, your doctor will order antibiotics that may be given by mouth or into a vein through an IV (intravenously). Sometimes more than one antibiotic is prescribed to help stop the infection.
How is VRE UTI treated?
Most VRE infections can be treated with antibiotics other than vancomycin. Laboratory testing can help healthcare providers determine which antibiotics will work. For people who have VRE infection in the bladder and a urinary catheter, removing the catheter when it is no longer needed can help get rid of the infection.
Does amoxicillin cover VRE?
For treatment of severe VRE infections, options include penicillin or amoxicillin +/– aminoglycoside, QPD, or newer agents such as LZD, daptomycin, and tigecycline.
What is the strongest antibiotic for MRSA?
Vancomycin or daptomycin are the agents of choice for treatment of invasive MRSA infections [1].
How is VRE diagnosed?
Tests and Diagnosis The only way to identify a VRE infection is to collect and test appropriate specimens in the laboratory. For example, a doctor might collect a urine sample for testing if he or she thinks a person has a urinary tract infection.
What is the difference between MRSA and VRE?
MRSA can be spread by touching articles that have been contaminated by the skin of an infected or colonized person, such as towels, sheets, and wound dressings; VRE can be transmitted by touching articles soiled by an infected person's feces.
How long does VRE last for?
The VRE germ can survive on hard surfaces for five to seven days and on hands for hours.
Does Levaquin cover VRE?
Bacteriostatic agent. Spectrum: covers all Gram positives including strep, MRSA and VRE.
What is the difference between MRSA and VRE?
MRSA can be spread by touching articles that have been contaminated by the skin of an infected or colonized person, such as towels, sheets, and wound dressings; VRE can be transmitted by touching articles soiled by an infected person's feces.
Why is VRE resistant to antibiotics?
Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them. If these germs develop resistance to vancomycin, an antibiotic that is used to treat some drug-resistant infections, they become vancomycin-resistant enterococci (VRE).
Is VRE infection curable?
You need to take the full course of antibiotics. VRE infections may be hard to cure. Bacteria do not respond to many antibiotics. You may need more than one antibiotic to stop the infection.
Does zosyn cover VRE?
Comparison of the 3 broadest spectrum beta-lactams: Cefepime, Zosyn, and Carbapenems (non-Ertapenem) have activity against both Gram positive (MSSA, Strep) and Gram negative including Pseudomonas. They do NOT cover: MRSA, VRE, Atypicals, among others.
What is CDC doing to address VRE infections?
This surveillance system collects reports of VRE from device-associated infections, such as central-line associated bloodstream infections.
How many deaths from VRE in 2017?
In 2017, VRE caused an estimated 54,500 infections among hospitalized patients and 5,400 estimated deaths in the United States [ Source: 2019 AR Threats Report ].
Why are enterococci resistant to antibiotics?
Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them.
What areas of the home can be contaminated with VRE?
frequently cleaning areas of the home, such as bathrooms, that may become contaminated with VRE
How are these infections treated?
In order to identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ. The provider will then select an antibiotic based on the activity of the antibiotic and other factors like potential side effects or interactions with other drugs.
What is the treatment for VRE?
Active VRE infections are treated with an antibiotic that’s not vancomycin. Your doctor can take a culture of the bacteria and have it tested in a laboratory to see which antibiotic might work best.
How to get rid of VRE?
Disinfect surfaces such as countertops and sinks that may have been contaminated with VRE. Wash dishes and utensils in warm, soapy water. Put bed linens and towels in the washing machine on hot. If you have to come into contact with open wounds or bodily fluids, always wear gloves.
How is VRE transmitted?
Most VRE infections are transmitted in hospitals. The bacteria often spread when a doctor or other healthcare worker touches an infected person, surface, or medical equipment and then doesn’t wash their hands properly before touching another patient.
What does VRE stand for?
Overview. VRE stands for vancomycin-resistant enterococcus. It’s an infection with bacteria that are resistant to the antibiotic called vancomycin. Enterococcus is a type of bacteria that normally lives in the intestines and the female genital tract. It usually doesn’t make us sick. However, sometimes it can cause infections in the: bloodstream.
Why is it so hard to treat a VRE?
These infections can be hard to treat because doctors have fewer options that are effective against the resistant bacteria. Some VRE infections may be life-threatening.
Where do most VRE infections occur?
Most VRE infections happen in people who are in the hospital. People who are infected often have a serious illness or weakened immune system.
Can you treat VRE with antibiotics?
Your outlook depends on what type of infection you have and your health in general. VRE can be somewhat challenging to treat because it’s resistant to vancomycin. However, other antibiotics can treat the infection.
What antibiotics are used for VRE?
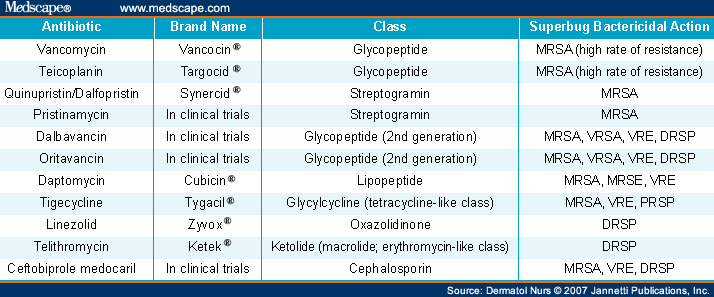
For VRE infections that cannot be managed with an aminopenicillin, the antibiotics daptomycin, linezolid, and tigecycline are three of the most common therapeutic options to consider. There are other drugs that have activity in vitro against VRE ( tedizolid, quinupristin/dalfopristin, fosfomycin, oritavancin, telavancin, chloramphenicol, ...
What is a VRE?
When vancomycin resistance is present , the organism is called a VRE. Approximately 80% of E. faecium and 5% of E. faecalis strains are vancomycin resistant [1]. Aminopenicillins can still be an option for ampicillin-sensitive VRE isolates. For VRE infections that cannot be managed with an aminopenicillin, the antibiotics daptomycin, linezolid, ...
What are the two most common enterococci?
The two most common species of enterococci to cause human infection are Enterococcus faecalis and Enterococcus faecium. Aminopenicillins ( e.g., ampicillin, amoxicillin) are widely considered the drugs of choice for infections caused by susceptible isolates, with vancomycin as a second-line drug. Both of these species can acquire vancomycin resistance through genes that cause peptidoglycan precursors to form that have decreased affinity for glycopeptide antibiotics like vancomycin. When vancomycin resistance is present, the organism is called a VRE. Approximately 80% of E. faecium and 5% of E. faecalis strains are vancomycin resistant [1]. Aminopenicillins can still be an option for ampicillin-sensitive VRE isolates.
Is VRE a problem?
When it comes to infections caused by Gram-positive bacteria, VRE are feared by many clinicians. In fact, VRE are so problematic that it was labeled a serious threat to human health by the United States Centers for Disease Control and Prevention in 2013. Unfortunately, it looks like VRE will be a problem for healthcare providers for many years to come yet.
How can VRE be transmitted?
There are reports that VRE can be transmitted by direct patient contact, touching of contaminated surfaces/equipment or through hand transfer after contact with the affected patient. In almost every hospital in the US, VRE has become a serious problem. In response to this epidemic, almost every hospital now has an infectious disease committee that oversees the use of antibiotics and audits procedures at the bedside for sterility. It is here that the role of the infectious disease nurse and pharmacist is vital. The current recommendations are to 1) only use vancomycin when absolutely needed, and permission must be obtained from the board-certified infectious disease pharmacist and clinician infectious disease specialist 2) educate all healthcare workers about VRE 3) implement infection control measures including hand washing, gloves, and gowns when coming into contact with patients who have VRE and 4) maintain a clean working environment with strict aseptic control. There is evidence to support the use of an interprofessional approach to prevent nosocomial spread of VRE. Many hospitals have now enforced the use of contact isolation and regular surveillance cultures. [17][18][19](Level V)
What are the risk factors for vancomycin-resistant Enterococcus?
The most commonly observed risk factor is previous antimicrobial therapy. This mechanism likely is due to alteration in bowel flora. Furthermore, patients at increased risk are those with severe underlying illnesses or immunosuppression. This also includes patients with a long hospital stay, admission to long-term care facilities, extended use of antibiotics, and proximity to other patients with vancomycin-resistant Enterococcus. [8][9]
What is tigecycline used for?
Tigecycline, a glycylcycline antibiotic, can be used for patients who are intolerant to other agents. It also can be used if other infections are present with the vancomycin-resistant Enterococcus as it has good coverage against gram positives, some gram negatives, and anaerobes. Although it is off-label, it is specifically considered a preferred agent for polymicrobial intraabdominal infections. It should not be used for vancomycin-resistant Enterococcus bacteremia as it distributes primarily to tissues and achieves low serum concentrations. Typical dosing is 100 mg IV once followed by 50 mg IV twice a day. Patients should be monitored for major adverse effects such as nausea and vomiting.
Is enterococcus a UTI?
Enterococcus is frequently cited as one of the three most likely etiologies of both uncomplicated and complicated UTI, especially health care-associated UTIs. Of these, the vast majority is E. faecalis, though the majority of vancomycin-resistant isolates are E. faecium. It is usually associated with indwelling urinary catheters and instrumentation. The severity of the disease can range from uncomplicated cystitis to complicated cystitis to pyelonephritis, perinephric abscess, or prostatitis. There is an increasing awareness that many reported “urinary tract infections” are, in fact, colonization. Asymptomatic pyuria and bacteriuria should not be treated unless the patient is exhibiting signs and/or symptoms of a UTI or sepsis.
Is vancomycin resistant enterococcus a challenge?
In particular, vancomycin-resistant Enterococcus (VRE) has become a challenge to manage in the hospital setting. Enterococci are facultative anaerobic gram-positive cocci in pairs/chains that live in the gastrointestinal (GI) tract and ordinarily function commensally with humans. However, they can cause a variety of infections, most commonly urinary tract infection (UTI), intraabdominal infection, bacteremia, or endocarditis. Rarely, they can cause meningitis, osteomyelitis, septic arthritis, or pneumonia. Additionally, vancomycin-resistant Enterococcus often exists as a colonizing organism that does not always contribute to infection, making it more difficult to determine when and how to treat these infections. Despite these difficulties, infection of vancomycin-resistant Enterococcus has been shown to increase both cost and mortality when compared to vancomycin-susceptible isolates. With increasing rates of vancomycin resistance among Enterococcus isolates, good stewardship combined with aggressive treatment with targeted antibiotics is necessary to treat this frequently encountered infection.[1][2][3]
Is VRE a problem?
Despite the proactive measures, VRE continues to be a problem in many hospitals. Short-term data show that the key to preventing VRE is the cautious use of the antibiotics and remaining compliant with infection control measures, especially in high-risk patients. [20][21](Level 5)
Is linezolid a bacteriostatic drug?
A synthetic oxazolidinone antibiotic, this is a bacteriostatic drug that binds to the ribosome, preventing peptide bond formation. For endocarditis, linezolid has been shown to be an effective first-line medication, although it is a bacteriostatic drug. Adverse effects, especially after prolonged use, include thrombocytopenia, anemia, peripheral neuropathy, and risk of inducing serotonin syndrome. Alternatives should be considered with patients who regularly take serotonergic medications.