What is the cause of diabetic ketoacidosis?
This usually occurs early on in life — childhood — but there are some subtypes that can occur in adults. We don't know the exact cause but there likely is an autoimmune aspect, where your body is attacking and destroying the beta cells of the pancreas ...
What are the signs of diabetic ketoacidosis?
The signs of diabetic ketoacidosis include:
- excessive thirst/drinking
- increased urination
- lethargy
- weakness
- vomiting
- increased respiratory rate
- decreased appetite
- weight loss (unplanned) with muscle wasting
- dehydration
- unkempt haircoat
Why is diabetic ketoacidosis so dangerous?
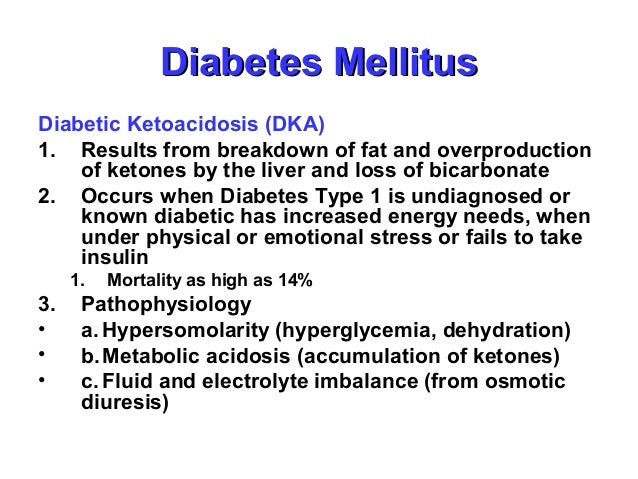
- Diabetic Ketoacidosis
- Diabetic Ketoacidosis Increases Risk of Acute Renal Failure in Pediatric Patients with Type 1 Diabetes
- Our Diabetes Story: My 11 Year old Son Went Into Diabetic Ketoacidosis and Was Diagnosed with Type 1 Diabetes
What you should know about diabetic ketoacidosis?
What You Should Know About Diabetic Ketoacidosis
- Testing for ketones. Testing for ketones is one of the first steps for diagnosing DKA. If you have type 1 diabetes, you should have a supply of home ketone tests.
- Preventing diabetic ketoacidosis. There are many ways to prevent DKA. ...
- Takeaway. DKA is serious, but it can be prevented. ...
Can diabetic ketoacidosis cause electrolyte imbalance?
In summary, hyperglycemia in DKA causes an osmotic diuresis, which results in severe fluid and electrolyte deficit.
Which electrolyte is most affected when the patient is in DKA?
Most of these effects are observed on CVS. First entity to get disturbed by the lack of insulin is electrolytes among which, potassium is most affected (6, 7).
What is associated with diabetic ketoacidosis?
You have many signs and symptoms of diabetic ketoacidosis — excessive thirst, frequent urination, nausea and vomiting, stomach pain, weakness or fatigue, shortness of breath, fruity-scented breath, and confusion.
Does DKA cause hypokalemia or hyperkalemia?
DKA is a well-known cause of hypokalemia caused by osmotic diuresis leading to a total body potassium deficiency of 3 to 6 mEq/kg. At presentation, potassium levels are typically “normal” due to the extracellular shift of potassium (K+) from insulin deficiency and acidosis.
What happens to sodium and potassium in DKA?
Potassium levels can fluctuate severely during the treatment of DKA, because insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity. A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis.
Why is potassium low in DKA?
Total body potassium depletion is expected in DKA largely due to osmotic renal losses.
What is the most common cause of ketoacidosis?
DKA is most common among people with type 1 diabetes. People with type 2 diabetes can also develop DKA. DKA develops when your body doesn't have enough insulin to allow blood sugar into your cells for use as energy. Instead, your liver breaks down fat for fuel, a process that produces acids called ketones.
Why is potassium high in DKA?
Insulin promotes potassium entry into cells. When circulating insulin is lacking, as in DKA, potassium moves out of cells, thus raising plasma potassium levels even in the presence of total body potassium deficiency [2,3].
Is sodium high or low in DKA?
In DKA, we expect to find normal or low serum sodium due to the dilutional effect of hyperosmolar status caused by elevated blood glucose that shifts water from the intracellular space to the extracellular space.
Does DKA cause hyperkalemia?
In DKA, the combination of insulin deficiency and the hyperglycaemia‐induced hyperosmolality frequently leads to hyperkalaemia, even though the patient may be markedly potassium‐depleted owing to potassium losses in the urine secondary to osmotic diuresis [1,2].
Why do you give potassium in DKA?
Replacement of potassium in intravenous fluids is the standard of care in treatment of DKA to prevent the potential consequences of hypokalemia including cardiac arrhythmias and respiratory failure.
How does ketoacidosis occur?
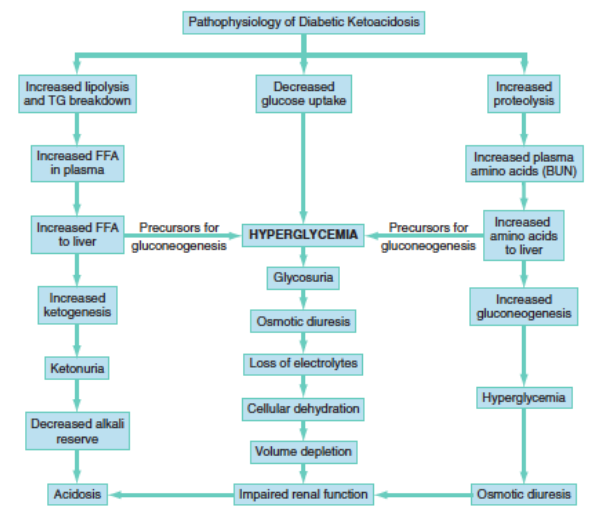
Diabetic ketoacidosis arises because of a lack of insulin in the body. The lack of insulin and corresponding elevation of glucagon leads to increased release of glucose by the liver (a process that is normally suppressed by insulin) from glycogen via glycogenolysis and also through gluconeogenesis. High glucose levels spill over into the urine, taking water and solutes (such as sodium and potassium) along with it in a process known as osmotic diuresis.[3] This leads to polyuria, dehydration, and polydipsia. The absence of insulin also leads to the release of free fatty acids from adipose tissue (lipolysis), which are converted through a process called beta oxidation, again in the liver, into ketone bodies (acetoacetate and β-hydroxybutyrate). β-Hydroxybutyrate can serve as an energy source in the absence of insulin-mediated glucose delivery, and is a protective mechanism in case of starvation. The ketone bodies, however, have a low pKa and therefore turn the blood acidic (metabolic acidosis). The body initially buffersthe change with the bicarbonate buffering system, but this system is quickly overwhelmed and other mechanisms must work to compensate for the acidosis. One such mechanism is hyperventilation to lower the blood carbon dioxide levels (a form of compensatory respiratory alkalosis). This hyperventilation, in its extreme form, may be observed as Kussmaul respiration..
What causes DKA in type 1 diabetes?
Triggers may include infection, not taking insulin correctly, stroke, and certain medications such as steroids.
What is the metabolic complication of diabetes?
Otherwise, scroll down to.Diabetic ketoacidosis is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with significant fluid and electrolyte loss.
Why do ketones show up in urine?
And when fat is broken down, ketones are released. These ketones will show up in the urine in a patient with diabetic ketoacidosis because there will be ketones circulating in the body. . 3.
What is the treatment for diabetic ketoacidosis?
Typical treatment regimens include crystalloid fluid therapy, insulin, and supplementation of dextrose, phosphorus, and potassium.
What causes hyperglycemia in diabetics?
1. Blood glucose level. During diabetic ketoacidosis, the body cells can’t use glucose for energy. This causes a build up of glucose in the blood, which leads to hyperglycemia (increased blood glucose).. 2.
Why do diabetics lose weight?
Untreated diabetic children, therefore, lose weight, are acidotic due to the buildup of ketone bodies in their blood (a state known as ketoacidosis), are dehydrated because of the loss of water, and experience an electrolyte imbalance because of the loss of electrolytes in urine.
What is HHNK and DKA?
DKA and HHNK are emergency conditions requiring quick medical care and nursing intervention. DKA can develop at any age and is most likely to occur in the insulin-dependent patient. The hallmark signs of DKA are a relative or absolute lack of insulin along with acidosis, ketosis, and hyperglycemia. Insulin and fluid and electrolyte therapy are ...
What is a DKA?
Fluid and electrolyte disorders associated with diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic coma. DKA and HHNK are emergency conditions requiring quick medical care and nursing intervention. DKA can develop at any age and is most likely to occur in the insulin-dependent patient. The hallmark signs of DKA are a relative ...
What are the symptoms of diabetic ketoacidosis?
The signs and symptoms of diabetic ketoacidosis include Risk factors for diabetic ketoacidosis are type 1 diabetes, and missing insulin doses frequently, or being exposed to a stressor requiring higher insulin doses (infection, etc).
What happens when your ketones are too high?
The buildup of ketones makes the blood more acidic. When the blood ketone level gets too high, a condition develops called diabetic ketoacidosis (DKA). It is a serious condition that can lead to coma or even death. DKA can happen to anyone with diabetes though it is more common in people with type 1 diabetes. [2] .
What is DKA in medical terms?
DKA is characterized by hyperglycemia, dehydration, ketonemia, metabolic acidosis and multiple electrolyte abnormalities. Treatment must be intensive and directed towards the correction of fluid, electrolyte and acid-base abnormalities as well as the correction of abnormal carbohydrate metabolism.
What is a DKA?
Diabetic ketoacidosis (DKA) is a medical emergency with a significant morbidity and mortality. It should be diagnosed promptly and managed intensively. DKA is characterised by hyperglycaemia, acidosis and ketonaemia: [1] Ketonaemia (3 mmol/L and over), or significant ketonuria (more than 2+ on standard urine sticks).
How do fatty acids convert to ketones?
These fatty acids are converted to ketones by a process called oxidation. The body consumes its own muscle, fat, and liver cells for fuel. In diabetic ketoacidosis, the body shifts from its normal fed metabolism (using carbohydrates for fuel) to a fasting state (using fat for fuel).
How much higher is the concentration of sodium in the serum than in the intracellular fluid?
For example, the concentration of sodium in extracellular fluid (serum) is about 15 times higher than in the intracellular fluid. Conversely, the concentration of potassium is about 30 times higher within the cell than in the serum or extracellular fluid. electrolyte imbalance.
What are the interactions between potassium and acid-base balance?
INTRODUCTION There are important interactions between potassium and acid-base balance that involve both transcellular cation exchanges and alterations in renal function [1]. These changes are most pronounced with metabolic acidosis but can also occur with metabolic alkalosis and, to a lesser degree, respiratory acid-base disorders. INTERNAL POTASSIUM BALANCE Acid-base disturbances cause potassium to shift into and out of cells, a phenomenon called "internal potassium balance" [2]. An often-quoted study found that the plasma potassium concentration will rise by 0.6 mEq/L for every 0.1 unit reduction of the extracellular pH [3]. However, this estimate was based upon only five patients with a variety of disturbances, and the range was very broad (0.2 to 1.7 mEq/L). This variability in the rise or fall of the plasma potassium in response to changes in extracellular pH was confirmed in subsequent studies [2,4]. Metabolic acidosis — In metabolic acidosis, more than one-half of the excess hydrogen ions are buffered in the cells. In this setting, electroneutrality is maintained in part by the movement of intracellular potassium into the extracellular fluid (figure 1). Thus, metabolic acidosis results in a plasma potassium concentration that is elevated in relation to total body stores. The net effect in some cases is overt hyperkalemia; in other patients who are potassium depleted due to urinary or gastrointestinal losses, the plasma potassium concentration is normal or even reduced [5,6]. There is still a relative increase in the plasma potassium concentration, however, as evidenced by a further fall in the plasma potassium concentration if the acidemia is corrected. A fall in pH is much less likely to raise the plasma potassium concentration in patients with lactic acidosis Continue reading >>
What are the precipitants of DKA?
Omission of insulin and infection are the two most common precipitants of DKA. Noncompliance may account for up to 44% of DKA presentations; while infection is less frequently observed in DKA patients.
How to prevent hypokalemia?
Hypoglycemia and hypokalemia are the most frequent complications and can be prevented by timely adjustment of insulin dose and frequent monitoring of potassium levels.
How to calculate anion gap acidosis?
Anion gap acidosis is calculated by subtracting the sum of Cl and HCO3 from measured (not corrected) Na concentration and should be corrected for hypoalbuminemia. Usually a HCO3 level of 18-20 meq/L rules out metabolic acidosis. Arterial blood gases with pH<7.30 support the diagnosis. β-OHB is early and abundant ketoacid and indicative of ketosis. Acetoacetate but not acetone, is a product of ketone body formation and is are measured by a majority of laboratories but may be negative in the blood in early DKA. Effective serum osmolality can be measured directly or derived from following formula: 2 x [measured Na+(meq/L)] + glucose/18. High measured Na indicates a significant degree of dehydration. A white blood cell count >25,000 should warrant a comprehensive search for infection. Serum creatinine can be falsely elevated because of acetoacetate interference with the colorimetric creatinine assay. When patients with DKA present with mixed acid-base disorder, measurement of serum β-OHB will be required to confirm that acidosis is due to ketoacidosis.
How does hyperglycemia evolve?
Hyperglycemiaof DKA evolves through accelerated gluconeogenesis, glycogenolysis, and decreased glucose utilization – all due to absolute insulin deficiency. Of note, diabetes patients who developed DKA while treated with SGLT-2 inhibitors can present without hyperglycemia, i.e., with euglycemic DKA. Due to increased lipolysis and decreased lipogenesis, abundant free fatty acids are converted to ketone bodies: β-hydroxybutyrate (β-OHB), acetoacetate, and acetone. Hyperglycemia-induced osmotic diuresis, if not accompanied by sufficient oral fluid intake, leads to dehydration, hyperosmolarity, electrolyte loss, and subsequent decrease in glomerular filtration. With decline in renal function, glycosuria diminishes and hyperglycemia/hyperosmolality worsens. With impaired insulin action and hyperosmolality, utilization of potassiumby skeletal muscle is markedly diminished leading to intracellular potassium depletion. Also, potassium is lost via osmotic diuresis causing profound total body potassium deficiency. Therefore, DKA patients can present with broad range of serum potassium concentrations. Nevertheless, a “normal” plasma potassium concentration may indicate that potassium stores in the body are severely diminished and the institution of insulin therapy and correction of hyperglycemia will lead to future hypokalemia.
How long does it take to replace DKA?
Fluid therapy: Replace fluid deficit in DKA (~6 L) within 24-36 hours with the goal of 50% volume replacement within first 12 hours.
What are the diseases of the cardiovascular system?
Acute medical illnessesinvolving the cardiovascular system (myocardial infarction, stroke, acute thrombosis) and gastrointestinal tract (bleeding, pancreatitis), diseases of endocrine axis (acromegaly, Cushing`s syndrome, hyperthyroidism) and impaired thermoregulation or recent surgical procedures can contribute to the development of DKA by causing dehydration, increase in insulin counterregulatory hormones, and worsening of peripheral insulin resistance.
What is cerebral edema?
Cerebral edema is reported in young adult patients. This condition is manifested by appearance of headache, lethargy, papillary changes, or seizures. Mortality is up to 70%. Mannitol infusion and mechanical ventilation should be used to treat this condition.
What are the mainstays of management in diabetic ketoacidosis?
Fluid resuscitation and maintenance, insulin therapy, electrolyte replacement, and supportive care are the mainstays of management in diabetic ketoacidosis.
What is the normal anion gap for diabetic ketoacidosis?
The normal anion gap is 12 mEq/l.
What is the incidence of DKA in children?
The highest incidence rate was found in Sweden and Finland, with 41.0 and 37.4 per 100,000.[6] In the United States, one study reported nursing home residents accounted for 0.7% of DKA. Increased mortality was associated with nursing home residence among patients with DKA.[7] Mortality rate greater than 5% has been reported in the elderly and patients with concomitant life-threatening illnesses. Death in these conditions is rarely because of the metabolic complications of hyperglycemia or ketoacidosis alone.
Why are elderly people at risk for hyperglycemia?
Some of the causes are increased insulin resistance and a decrease in the thirst mechanism. The elderly are particularly vulnerable to hyperglycemia and dehydration, the critical components of hyperglycemic emergencies. With increased diabetes surveillance and aggressive early treatment of hyperglycemia and its complications, morbidity, and mortality from acute diabetic crises in the geriatric population can be significantly reduced. [11]
What is DKA in medical terms?
Diabetic ketoacidosis (DKA) is characterized by uncontrolled hyperglycemia, metabolic acidosis, and increased body ketone concentration. It is a life-threatening complication of diabetes and is usually seen in patients with type-1 diabetes mellitus. Rarely it may also occur in patients with type-2 diabetes mellitus. ...
How does insulin affect diabetes mellitus?
Insulin decreases hepatic glucose production by inhibiting glycogenolysis and gluconeogenesis. Glucose uptake by skeletal muscle and adipose tissue is increased by insulin. Both of these mechanisms result in the reduction of blood sugar. In diabetic ketoacidosis, insulin deficiency and increased counter-regulatory hormones can lead to increased gluconeogenesis, accelerated glycogenolysis, and impaired glucose utilization. This will ultimately cause worsening hyperglycemia.
Why is DKA recurrent?
One of the major causes of recurrent DKA in the inner-city population in the United States is non-compliance with insulin. Socioeconomic and educational factors play a significant role in poor adhesion to medications, including insulin. A recent report suggests that cocaine abuse is an independent risk factor associated with DKA recurrence. [4]
