Does type AB have no antigens?
Antigens are surface proteins found on red blood cells. Type O negative blood is the only blood type with no antigens. Blood type A has an A antigen, while blood type B has a B antigen. Blood type AB has both A and B antigens.
What blood type has neither antibodies?
Type O-negative blood does not have any antigens. It is called the "universal donor" type because it is compatible with any blood type. Type AB-positive blood is called the "universal recipient" type because a person who has it can receive blood of any type.
Why a person with type AB blood would not have anti-A or anti-B antibodies in their plasma?
Those who have type AB blood do not make any ABO antibodies. Their blood does not discriminate against any other ABO type. Consequently, they are universal receivers for transfusions, but their blood will be agglutinated when given to people with every other type because they produce both kinds of antigens.
What is unique about AB blood type?
AB positive blood type is known as the “universal recipient” because AB positive patients can receive red blood cells from all blood types.
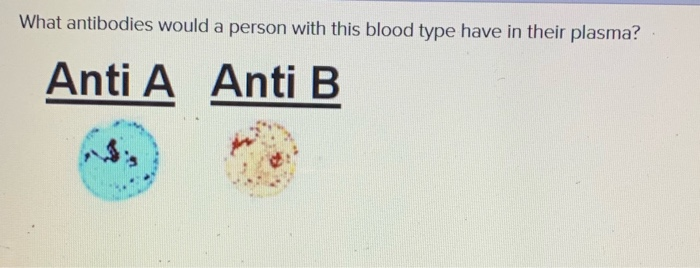
What antibodies are in type AB blood?
blood group AB – has both A and B antigens, but no antibodies.
What is the golden blood type?
One of the world's rarest blood types is one named Rh-null. This blood type is distinct from Rh negative since it has none of the Rh antigens at all. There are less than 50 people who have this blood type. It is sometimes called “golden blood.”
Why AB is called universal recipient?
Individuals with the AB blood group are known as universal recipients because they can receive blood from all blood kinds without experiencing any hemolytic reactions.
Why is AB the universal plasma donor?
It is enriched in proteins that help fight infection and aid the blood in clotting. AB plasma is plasma collected from blood group AB donors. It is considered "universal donor" plasma because it is suitable for all recipients, regardless of blood group.
Does AB negative have Rh antibodies?
Red blood cells (RBCs): Type AB Positive (left) and type AB Negative (right). Both types have A and B antigens, but only the AB Positive (left) has the Rh antigen....DonorRecipientAnti-Rh Antibodies in Recipient's BloodRh NegativeRh PositiveWill Not Produce anti-Rh Antibodies1 more row
What are the 3 rarest blood types?
The rarest blood types are: B negative(B -ve), which is found in 1.5 percent of the total population. AB negative(AB -ve), which is found in 0.6 percent of the total population. AB positive(AB +ve), which is found in 3.4 percent of the total population.
What ethnicity has AB blood type?
Distribution of blood types in the United States as of 2021, by ethnicityCharacteristicO-positiveAB-positiveCaucasian37%3%African American47%4%Asian39%7%Latino-American53%2%Oct 14, 2021
Which is the strongest blood group?
Type O negative red blood cells are considered the safest to give to anyone in a life-threatening emergency or when there's a limited supply of the exact matching blood type. That's because type O negative blood cells don't have antibodies to A, B or Rh antigens.
Is O+ blood type rare?
38% of the population has O positive blood, making it the most common blood type. O positive red blood cells are not universally compatible to all types, but they are compatible to any red blood cells that are positive (A+, B+, O+, AB+).
What are the 3 rarest blood types?
The rarest blood types are: B negative(B -ve), which is found in 1.5 percent of the total population. AB negative(AB -ve), which is found in 0.6 percent of the total population. AB positive(AB +ve), which is found in 3.4 percent of the total population.
Is O negative or O positive rare?
Only 7% of the population are O negative. However, the need for O negative blood is the highest because it is used most often during emergencies. The need for O+ is high because it is the most frequently occurring blood type (37% of the population).
Is O negative blood worth?
O negative blood is valuable because it can be transfused to anyone, regardless of their blood type. Hospitals need to have it on hand for emergencies. In addition, emergency services, including ambulances and helicopters, may also carry it to keep patients alive while they're being transported to a hospital.
What does AB mean in blood?
Antigens (on the surface of the red blood cells): AB indicates that both antigens A and B are present (if all possible antigens are present, antigens A, B and Rh, there are no antibodies in your blood plasma). AB Rh + blood type notation indicates which antigens and antibodies are present in the blood.
Which type of blood has antigens and produces B antibodies?
Type A blood has A antigens and produces B antibodies.
What is the blood group of a person?
Blood group of any person depends on the type of antigen ( these are proteins that are expressed on the surface of RBCs) that may be eiher A, or B, or can be AB i.e both A and B antigens expresses independently on RBC surface (codominance). And the type of antigen one expresses is genetically determined. Also, there are antibodies in the plasma that are against the opposite antigen which RBCs don't possess . In simple words, if a person has A blood group, then antibodies in his plasma would be against B ,ie anti- B antibodies (if this person is by mistake transfused with blood having B group a
Does blood have anti-A and anti-B antibodies?
The plasma of AB group blood do not contain the antibodies anti-A & anti-B. But A group and B group contains anti-B and anti-A antibodies respectively. The O group do have both A & B antibodies in the plasma. The antigens on the red cells are inherited and the antibodies concerned are natural and IgM type. When there is any inherited antigen present in the blood the immune system can not produce the specific antibodies that can appear in the plasma. The gut bacteria (commensals, normal flora) that posses a substance on their structure have the same human blood group ABO specificity. When the blood group antigens A & B are not inherited (group O), the immune system may respond to A & B substance of the gut bacteria to produce anti-A & anti-B antibodies in the plasma. This function starts in the body from 5–6 months of age until the end of life. When A & B antigens are present (AB group) the immune system can not respond to produce the antibodies. The groups A & B can not have the corresponding antibodies but the immune system can produce the antibodies based on the presence of specific substance on the gut bacteria and the absence of inherited antigen.
Does blood have antibodies?
The plasma of AB group blood do not contain the antibodies anti-A & anti-B. But A group and B group contains anti-B and anti-A antibodies respectively. The O group do have both A & B antibodies in the plasma. The antigens on the red cells are inherited and the antibodies concerned are natural and IgM type. When there is any inherited antigen present in the blood the immune system can not produce the specific antibodies that can appear in the plasma. The gut bacteria (commensals, normal flora) that posses a substance on their structure have the same human blood group ABO specificity. When the bl
Can plasma be given to anyone?
Incidentally, an O individual's plasma would contain antibodies against A and B antigens. Their plasma cannot be given to just anyone.
Can blood transfusions be tested for antigens?
They can theoretically accept types A, B, AB and O blood transfusions, BUT those are not the only blood cell antigens for which blood is tested. Blood transfusion is a whole subspecialty of pathology and laboratory medicine.
Which blood group has no antigens?
Similarly, blood group B has only B antigens, blood group AB has both, and blood group O has neither A nor B antigens on the surface of the red blood cells. These four groups are the most important because they indicate which blood type a patient can safely receive in a transfusion.
What does it mean when your blood is positive?
Meanwhile, your blood is either “positive,” meaning it contains the Rhesus D antigen, or “negative” meaning it lacks it. This is another inherited blood marker that also matters when it comes time for a transfusion.
What are the markers on the surface of red blood cells?
On the surface of the red blood cells, as Silberstein explained, are proteins with attached carbohydrates, essentially markers that identify the blood cells as our own. These microscopic markers, known as antigens, are commonly grouped in eight basic blood types: A, B, AB, and O, each of which can be either “positive” or “negative.”.
How many red blood cells are there in the human body?
Red blood cells, manufactured in the bone marrow, perform the hard work of carrying oxygen around the body. In every two to three drops of blood, roughly one billion blood cells reside. Red cells far outnumber both the platelets, which stop bleeding by clotting blood vessel injuries, and white cells, which protect your body from pathogens and disease. For every 600 red blood cells there are a mere 40 platelets and just one solitary white blood cell.
What are the components of blood?
All blood contains the same basic components: red cells, white cells, platelets, and plasma, which is the liquid portion of blood holding the red and white blood cells along with the platelets in suspension. We inherit blood group genes from our parents, with odds of receiving one A and one B gene lower than other possible combinations.
Which blood group is more prevalent in Asians compared to Caucasians?
For example, blood group B is more prevalent in Asian individuals compared to Caucasians, while Group O is more common in Hispanics. Based on the population as a whole, though, these are the approximate proportions.
Can you receive blood if you are AB positive?
In the case of blood types, being the rare one offers one huge advantage: people who are AB positive can receive any blood type and so are known as “universal recipients.”. If you’re more of a giver, though, you’d much rather have O negative blood.
How many alleles are there in the ABO blood group?
There are three alleles responsible for four main ABO blood group system phenotypes. The phenotypes produced are A, B, AB, and O. The carbohydrates defining A and B antigens are added to the H antigen, fucose ( Fig. 6-1 ). Together there are more than 90 alleles of the three major gene blood types. The origin of these alleles is the gene producing a glycosyltransferase enzyme that attaches a sugar to a precursor.
What are the four blood groups in the ABO system?
The ABO blood group system has four distinct phenotypes: A, B, AB, and O. Red cells with the blood groups A, B, and AB carry distinct carbohydrate antigens on their surface; red cells with blood group O carry none. The plasma carries ABO red cell antibodies or agglutinins that are specific for the ABO blood antigens that are lacking.
What are the four blood groups?
There are four major blood groups, A, B, AB, and O , determined by the presence or absence of A and B antigens on the surface of RBCs. Group A has only A antigen, group B carries B antigen, and group AB has both A and B antigens on the RBCs. Group O has neither A nor B antigen, but group O individuals have H antigen, which is the precursor substrate for A and B antigens. The A and B antigens are synthesized by transferase enzymes and differ only by the nature of the terminal carbohydrate to a d -galactose (Gal) residue that also has l -fucose (Fuc) in a 1-2 linkage of the N-linked oligosaccharides chain. N -acetyl- d -galactosamine is added by A-transferase, and d -galactose by B-transferase. Group O individuals have defective A or B transferases; therefore, no terminal carbohydrate is added, leaving H antigen, the terminal sugar of which is fucose, on the RBC. Some H antigen precursor remains on A and B RBCs in this order: A2 > B > A 2 B > A 1 > A 1 B. In clinical practice, four ABO phenotypes (A, B, O, and AB) are discriminated. In addition, two common variations of group A, A 1, and A 2, can be distinguished. A 1 and A 2 phenotypes differ in the amount of A antigen on the RBCs (A 2 has less than A 1) and differ in carbohydrate branching structure. Approximately 80% of group A individuals are A 1 and 20% are A 2. In addition, there are other inherited phenotypes that have weaker expression of the specified antigen, e.g., A 3, Ax, Ae l, B 3, B (A), and cisAB.
How is blood group chimerism created?
There are several ways in which blood group chimerism may be created: through inheritance of more than one cell lineage in embryonic development or through medical therapy. No matter what the mechanism, blood group chimerism will often be detected when testing the blood for the purposes of medical care, usually in preparation for a blood transfusion. If more than one red blood cell population is encountered, an investigation to determine the underlying cause is necessary. Discrepant results in the blood bank can delay the availability of blood for transfusion.
What is acquired blood group chimerism?
Acquired Blood Group Chimerism. Acquired blood group chimerism is medically induced and can be a transient phenomenon or a permanent state. Transient blood group chimerism is the most common type of blood group chimerism. It happens following transfusion of ABO-compatible, but not ABO-specific, red blood cells.
What is the relationship between ABH and breast cancer?
One hundred sixty-six female patients with breast cancer were examined. They revealed that blood group A is more often associated with ductal breast cancer (49.6%), in contrast to the other blood groups, and particularly to blood group AB (3.6%). The relative risk of metastasis in Rh (−) patients was 4.2 times higher than that in Rh (+) patients. Consequentially, blood group A, and particularly A (−), has the worst prognosis of all.126
What is the biological compatibility of blood transfusion?
This biological compatibility allows patients in need of emergent transfusion, such as after a traumatic event, to safely receive blood group O cells (universal donor). This is standard practice for hospitals treating trauma victims. Following ABO-compatible (but not identical) transfusion, patients with A, B, or AB blood types will display more than one blood type when tested; thus, a blood group chimera is transiently created. As the transfused red cells live their normal life span of approximately 120 days, they will be removed from circulation and the patient will return to their natural blood type. Genetic testing of the patient during this time can elucidate the patient’s true ABO blood type, if it is necessary to determine for the purposes of clinical care.
What is the ABO blood type?
The ABO blood typing is a naming scheme that states the presence or absence of just two antigens: antigen A and antigen B. The antigens that are present on the surface of our red blood cells determine our blood type.
What determines blood type?
TL; DR. Blood type is determined by which antigens present on red blood cells. Antigens are macromolecules (usually proteins) that can elicit an immune response and help the body determine ‘self’ vs. ‘foreign’. Antibodies recognize antigens and target them for degradation.
What happens to erythrocytes after infusion?
Following an infusion of incompatible blood, erythrocytes with foreign antigens appear in the bloodstream and trigger an immune response. Proteins called antibodies would then attach to the antigens on the plasma membranes of the infused erythrocytes and cause them to adhere to one another.
How many antigens are on erythrocyte membranes?
More than 50 antigens have been identified on erythrocyte membranes, but the most significant in terms of their potential harm to patients are classified in two groups: the ABO blood group and the Rh blood group
What is an antigen?
An antigen is a foreign or “non-self” macromolecule (typically a protein) that reacts with cells of the immune system. However, not all antigens will provoke a response. For example, each of us produce a large number of self-antigens.
Can you have an antibody with type A blood?
Normally the body must be exposed to a foreign antigen before an antibody can be produced. This is not the case for the ABO blood group. Individuals with type A blood—without any prior exposure to incompatible blood—have preformed antibodies to the B antigen circulating in their blood plasma. These antibodies, referred to as anti-B antibodies, will cause agglutination and hemolysis if they ever encounter erythrocytes with B antigens. Reviewing thelook at the table below:
When was blood transfusion discovered?
Blood transfusions in humans were risky procedures until the discovery of the major human blood groups by Karl Landsteiner, an Austrian biologist and physician, in 1900. Until that point, physicians did not understand why death sometimes followed blood transfusions when a donor’s blood infused into the patient was incompatible with ...
How do B lymphocytes produce antibodies?
1. Antibody-producing cells (B lymphocytes) generate antibodies through a gene recombination process, that allows a virtually infinite number of antibodies to different antigens to be created, including against self-antigens ( https://en.wikipedia.org/wiki/V (D)J_recombination ).
Do people with type O blood have anti-A and anti-B antibodies?
People with type O blood have anti-A and anti-B antibodies, even without receiving a transfusion. Why?
Does O blood have antigens?
Likewise, someone with an O type blood won't have both the A and B antigens, and so cells producing antibodies that bind to them will be allowed to mature, and they will have anti-A and anti-B antibodies circulating in the blood.
Do we have antibodies for self-antigens?
If we do encounter them, then the cells that produce those antibodies will multiply and the number of those antibodies will greatly grow. Typically , we only don't have antibodies for self-antigens.