How Do Vets Calculate Fluid Therapy? Vets calculate how much fluid to give animals by estimating the total body water within a healthy animal of that size, then determining the deficit. Dogs and cats typically have an average body water of about 60% of their body weight.
How do you calculate fluid per kg of blood?
1) Daily volume formula: (100 mL for each of the first 10 kg) + (50 mL for each kg between 11 and 20) + (20 mL for each additional kg past 20 kg) = 1,000 mL + 500 mL + 120 mL = 1,620 mL. Fluid rate = 1,620 / 24 = 68 mL (67.5). 2) 4 – 2 – 1 rule:
How do you calculate pediatric maintenance fluid rate?
These are the two methods for calculating pediatric maintenance fluid rates, applied in the case of a child weighing 26 kg. 1) Daily volume formula: (100 mL for each of the first 10 kg) + (50 mL for each kg between 11 and 20) + (20 mL for each additional kg past 20 kg) = 1,000 mL + 500 mL + 120 mL = 1,620 mL.
How do you calculate fluid loss from dehydration?
Body weight in kg x percent dehydration (as a decimal) = the fluid deficit in ml Body weight in lb x percent dehydration (as a decimal) x 500 = fluid deficit in ml The two categories of ongoing fluid loss include sensible and insensible losses. Sensible losses are those that can be quantified ( e.g. urination).
How to calculate the daily volume of fluid maintenance?
In order to calculate the daily volume, the following formulas are applied: Weight Fluid Maintenance By Holliday-Segar Nomo ... 3.5 – 10 kg 100 mL/kg >10 – 20 kg 100 mL/kg for the first 10 kg, then 50 m ... >20 – 65 kg 1500 mL plus 20 mL for each kg past 20 k ... >65 kg 2400 mL

How do you calculate patient fluid?
Maintenance Fluid Rate is calculated based on weight.4 mL / kg / hour for the first 10kg of body mass.2 mL / kg / hour for the second 10kg of body mass (11kg - 20kg)1 mL / kg / hour for any kilogram of body mass above 20kg (> 20kg)
How do you calculate IV fluid intake?
1:2512:56Intravenous fluid calculations | IV Drip rate Calculations | Drops/minuteYouTubeStart of suggested clipEnd of suggested clipThis is calculated by a simple formula ml per hour equal to total infusion volume in ml divided byMoreThis is calculated by a simple formula ml per hour equal to total infusion volume in ml divided by total infusion.
How do you calculate rehydration fluid?
Deficit (mL) = weight (kg) x % dehydration x 10 In the first 24 hours replace 5% dehydration. For this infant that is 500 mL (ie 500 mL ÷ 24 = 20.5 mL/hr). Replace the remaining deficit (here another 500 mL ÷ 24 = 20.5 mL/hr) if still indicated after clinical reassessment, over the following 24 hours.
How do you calculate IV fluids for adults?
The 24-hour number is often divided into approximate hourly rates for convenience, leading to the "4-2-1" formula.100 ml/kg/24-hours = 4 ml/kg/hr for the 1st 10 kg.50 ml/kg/24-hours = 2 ml/kg/hr for the 2nd 10 kg.20 ml/kg/24-hours = 1 ml/kg/hr for the remainder.
How do you calculate fluid intake and output?
Intake and output (I&O) is the measurement of the fluids that enter the body (intake) and the fluids that leave the body (output). The two measurements should be equal. (What goes in…. must come out!)...Conversions:1 cc. = ml.2 oz. = ml.½ oz. = ml.4 cc. = ml.8 oz. = ml.6 oz. = ml.4 oz. = ml.½ cup = oz. = ml.More items...
How do you calculate IV fluid hours?
The formula to calculate how many hours will it take for the IV to complete before it runs out is: Time (hours) = Volume (mL) Drip Rate (mL/hour) .
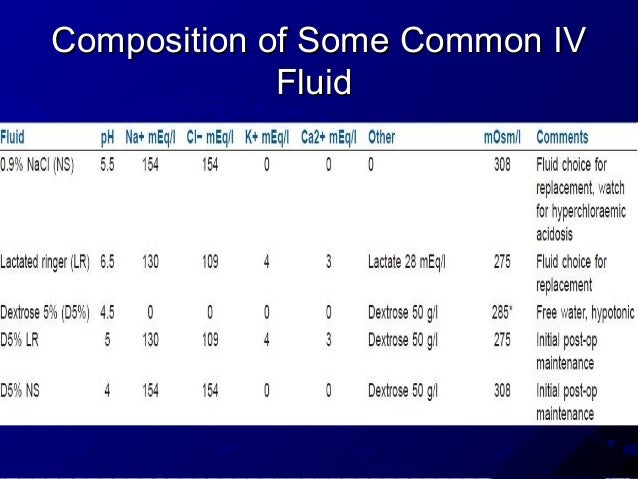
What are the 5 R's of fluid therapy?
When prescribing IV fluids, remember the 5 Rs: Resuscitation, Routine maintenance, Replacement, Redistribution and Reassessment.
What is a normal IV fluid rate?
Normal daily fluid and electrolyte requirements: 25–30 ml/kg/d water 1 mmol/kg/day sodium, potassium, chloride 50–100 g/day glucose (e.g. glucose 5% contains 5 g/100ml). Stop IV fluids when no longer needed. Nasogastric fluids or enteral feeding are preferable when maintenance needs are more than 3 days.
How do I calculate flow rate?
How to calculate flow rate? Flow rate formulasVolumetric flow rate formula: Volumetric flow rate = A × v. where A - cross-sectional area, v - flow velocity.Mass flow rate formula: Mass flow rate = ρ × Volumetric flow rate = ρ × A × v. where ρ – Fluid density.
How is fluid target calculated for elderly?
A formula used to calculate fluid requirements for older people is: U 100 mL fluid per kg body weight for the first 10 kg U 50 mL fluid per kg for the next 10 kg U 15 mL fluid per kg for each kg after 20 kg.
How do you calculate pediatric fluids?
Daily fluid requirements. ... Fluid requirements per hour: Daily fluid requirements are divided into approximate hourly rates which gives the "4-2-1" formula often used to calculate hourly infusion rates of IV fluids. ... Example: A 35 kg child minimum hourly fluid intake would be: (4x10) + (2x10) + (1x15) = 75 cc/hour.Table 2.
What does 5% dehydration mean?
Severely reduced. When we talk of "5% dehydration", it means that the child has lost an amount of fluid equal to 5% of the body weight. If you have an accurate pre-illness weight, you may use that weight.
Comprehensive Plan
Calculates fluid required to provide maintenance requirements, correct dehydration and replace ongoing losses.
Simple Rate Calculator
Useful for calculating fluid rates for resuscitation, and fluid rates for large animals.
What is the requirement for IV fluids calculator?
The only requirement in the IV maintenance fluids calculator is to input the weight of the pediatric patient in either kg or lbs. Given that the formulas use kg as standard weight unit, lbs will be transformed to kg.
How does this IV maintenance fluids calculator work?
This health tool estimates the fluid requirement in the case of pediatric patients based on the formulas beyond the Holliday-Segar nomogram and the 4 – 2 – 1 rule.
Why is fluid therapy important?
Fluid therapy is instituted in order to preserve the normal volume of body fluids and their electrolyte composition. The two components are homeostasis preserving maintenance and repletion.
What is the most common cause of dehydration in pediatric patients?
The most common cause of dehydration in pediatric patients is diarrheal fluid loss. In these cases, depending on the maintained serum sodium level (normal range between 135 – 145 mEq/L), electrolyte loss can vary from isotonic to hypo-osmolar.
How much water is needed to replace insensible water loss?
As a rule of thumb, water loss (and water requirement) is function of caloric expenditure and the total daily water requirement to replace insensible and urinary water loss in hospitalized patients is approximately 100 mL/ 100 kcal/day.
Does fluid loss occur in infants?
Usually fluid loss takes place at a normal rate, however, febrile infants and children have a greater transcutaneous evaporative water loss.
How to determine fluid status?
Often, one can determine the patient’s fluid status clinically based on a variety of physical exam findings and objective data from their vital signs. Laboratory markers are helpful as adjunctive data. The following is a list of findings that can help determine whether a patient is fluid-depleted or volume overloaded. [1]
How to measure volume changes in a patient?
Weight: One of the most sensitive indicators of patient volume status changes is their body weight. Patient weight changes approximate a gold standard to determine fluid status. Unfortunately, due to differences in scales available to hospital staff, this can be a challenging target to measure. It is ideal to weigh a patient daily on the same scale to determine trends in weight changes. One can see weight gain in states of fluid excess and weight loss in states of fluid deficit. It is also helpful to look at patient records to see any recent outpatient visits before hospitalization, which might indicate a patient's normal baseline weight.
What is the difference between maintenance fluids and fluid replacement?
Maintenance fluids should address the patient's basic physiologic needs, including both sensible and insensible fluid losses. Sensible fluid losses refer to typical routes of excretion such as urination and defecation. Insensible losses refer to other routes of fluid loss, such as in sweat and from the respiratory tract. Fluid replacement goes beyond the normal physiologic losses and includes such conditions as vomiting, diarrhea, or severe cutaneous burns. One must consider these 2 categories of fluid loss separately when devising a fluid management strategy for an individual patient.
What is fluid management?
Fluid management is a critical aspect of patient care, especially in the inpatient medical setting. What makes fluid management both challenging and interesting is that each patient demands careful consideration of their individual fluid needs.
How long does it take for a capillary to refill?
Capillary refill: Normally less than 2 seconds. Easy to test on fingertips and toes
Is there a standardized guideline for adult maintenance intravenous therapy?
One must exercise caution in applying these weight-based formulae to patients who are elderly or obese.[3] Unfortunately, no standardized guidelines exist at this point to guide adult maintenance intravenous therapy. It is beyond the scope of this article to delve into the nuances of deciding between various tonicities and volumes of fluid administration. These choices demand clinical judgment based on the initial fluid status of the patient and predictions of ongoing fluid needs. The electrolyte derangements discussed below in the complications section show potential issues arising from certain fluid choices.
Can you see weight gain in fluid deficit?
One can see weight gain in states of fluid excess and weight loss in states of fluid deficit. It is also helpful to look at patient records to see any recent outpatient visits before hospitalization, which might indicate a patient's normal baseline weight.
What is the best fluid to add to electrolytes?
Use saline or a balanced electrolyte fluid, then add required electrolytes. Saline is typically reserved for patients with a sodium level less than 125mEq/l, in disease states such as high potassium, HYPP or renal failure. Long term fluids- need to add potassium, magnesium and calcium for maintenance.
How much water does a horse have?
The body of an adult horse contains about 60% water which is divided into the extracellular (1/3) and intracellular spaces (2/3). In neonates the percentage of body weight made up of water is even higher (75-85%). The intravascular space only makes up 5% - 8 % of the horse’s body weight (10% - 15% in foals). By 12 weeks of age the foal’s water distribution more closely resembles the adult. Potassium and magnesium high intracellularly while sodium, chloride and bicarbonate are higher in the extracellular fluid (95% of the body’s sodium). Low calcium and magnesium are common in horses with surgical colic or colitis.