Peritonitis rates may be calculated in 1 of 2 ways: 1. Months of peritoneal dialysis at risk (ie total number of months each patient has spent on dialysis), divided by number of episodes (ie total number of episodes experienced by all patients), and expressed as interval in months between episodes (eg 1 per 20 patient-months); or, 2.
How do you calculate peritonitis rate?
1 answer. Peritonitis rates may be calculated in 1 of 2 ways: 1. Months of peritoneal dialysis at risk (ie total number of months each patient has spent on dialysis), divided by number of episodes (ie total number of episodes experienced by all patients), and expressed as interval in months between episodes (eg 1 per 20 patient-months); or,
How is peritonitis diagnosed in peritoneal dialysis patients?
As a peritoneal dialysis patient, it’s important to know the signs and symptoms of peritonitis. If you experience any of the following, contact your doctor immediately. Your doctor may be able to diagnose peritonitis based on your signs and symptoms and status as a peritoneal dialysis patient.
How is peritonitis treated in patients on continuous ambulatory peritoneal dialysis (CAPD)?
Between 1977 and 1978, the peritonitis rate in patients on continuous ambulatory peritoneal dialysis (CAPD) using bottles was 5.5 episodes per year at risk. Treatment was intraperitoneal cefazolin at 125 mg/L dialysis fluid. An aminoglycoside (gentamicin or tobramycin) was added at a dose of 4–8 mg/L if Gram-negative infection was suspected.
How many episodes of peritonitis per patient year?
Example: 2 episodes peritonitis/5.5 patient years = 0.36 episodes per patient year Include hospital days (once home therapy begins) in total days at risk Include hospital acquired peritonitis (once home therapy begins) in total peritonitis rate 2
METHOD 1: Peritonitis Rate: One episode per number of patient months 1
Total number CAPD/APD patient days at risk/30.4 days per month = patient months experience
METHOD 2: Peritonitis Rate: Episodes per patient year 1
Total number CAPD/APD patient days at risk/365 days per year = patient years experience
Important points
Include hospital days (once home therapy begins) in total days at risk
How long does it take to treat polymicrobial peritonitis?
The patient should be treated with effective antibiotics for 3 weeks.
What is the treatment for tuberculous peritonitis?
Special culture techniques should be considered. Treatment should be based on a 4 drug regimen: rifampicin, isoniazid, pyrazinamide, and ofloxacin, if diagnosed. Pyraz inamide and ofloxacin can be stopped after 2 months but rifampin and isoniazid should be continued for a total of 12 to 18 months. Patients often respond to therapy without catheter removal.
What is peritoneal dialysis?
Introduction to Peritonitis in Peritoneal Dialysis. Peritonitis is the inflammation of the peritoneum or peritoneal membrane. This type of inflammation typically has an infectious etiology that is mainly caused by bacteria (~80% of cases). Bacterial infections mainly come from contamination during a peritoneal dialysis (PD) session.
What is the most common complication of PD?
Peritonitis is a major complication of PD due to the structural changes in the peritoneal membrane that result from PD. Approximately 4% of peritonitis episodes result in death. Since peritonitis is one of the more common complications of PD, it has caused patients to switch from this modality to hemodialysis.
Why is culture negative for peritonitis?
Culture negative peritonitis may be due to recent antibiotic usage or technical reasons. The guidelines recommend repeat WBC count with differential if the effluent yields no growth after 3 days. If the peritonitis has not clinically improved at day 3, special culture techniques that test for mycobacteria, nocardia, legionella, filamentous fungus, or other fastidious bacteria should be considered. Initial therapy may be continued for 2 weeks if clinical improvement is noted and the effluent clears quickly. However, if improvement is not observed in 5 days, catheter removal should be strongly considered.
Why is monitoring peritonitis important?
Monitoring peritonitis rates and evaluating outcomes of peritonitis treatment are important to ensure patients are receiving the best possible treatment.
How long after refractory peritonitis can you take antibiotics?
Simultaneous re-insertion of a new catheter is not recommended for refractory and fungal peritonitis. Antibiotics should be continued for at least 2 weeks after catheter removal for refractory peritonitis.
How to prevent peritonitis from PD?
If you are a peritoneal dialysis patient, prevent peritonitis by following these steps: (iii) Keep the skin around your PD catheter clean and check for redness, drainage, or swelling. Wash or sanitize your hands before touching the catheter.
What causes Peritonitis in Peritoneal Dialysis patients?
Peritonitis is a peritoneal dialysis-related infection caused by bacteria entering the abdomen from outside the body and infecting the peritoneum. Bacteria may enter the body through the open ends of the PD catheter during exchanges. If you touch your PD catheter cap, bacteria from your fingers may transfer onto the catheter and enter the peritoneum. (iii) Peritonitis can also occur if there is PD catheter exit site infection or tunnel infection.
What is the peritoneum associated with?
Understanding Peritonitis Related to Peritoneal Dialysis. Peritonitis is one of the few complications associated with peritoneal dialysis . The peritoneum is the thin membrane that lines your abdominal cavity and covers the organs contained within it. Peritonitis is the inflammation of this membrane. Although peritonitis can result ...
How long do peritoneal dialysis catheters work?
With appropriate catheter placement and exit-site care, most peritoneal dialysis catheters are problem-free and work well for years.
How do you know if you have peritoneal dialysis?
If you experience any of the following, contact your doctor immediately. Abdominal pain. Fever, nausea, or vomiting. Cloudy dialysis fluid when drained from your body. Sore or swollen abdomen.
Why is it important to take care of a PD catheter?
Care of the catheter and the skin around the catheter (called the catheter exit site) is very important in maintaining PD catheter function and to minimize the risk of developing an infection.
Can you get dialysis for peritonitis?
Catheter removal is also a consideration if you have had repeated bouts of peritonitis. Your doctor may recommend that you receive dialysis in an alternate way until your body recovers from the infection. In any case, your physician will know the best approach for your situation. (iii)
What is the plague of peritoneal dialysis?
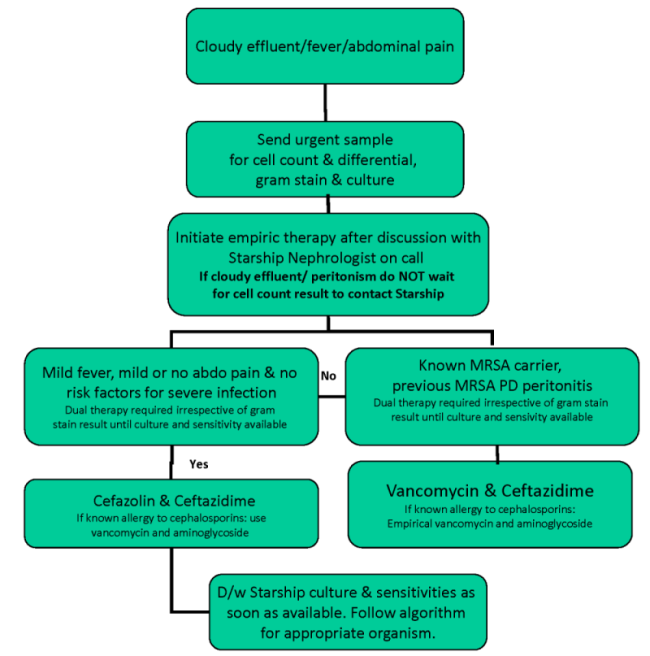
Peritonitis has been the plague of patients on peritoneal dialysis (PD) since its inception. In an early article by the PD pioneer Karl Nolph and coworkers ( 1 ), peritonitis was defined as cloudy effluent with 100 white cells per millimeter, of which 50% were polymorphonuclear cells. Between 1977 and 1978, the peritonitis rate in patients on continuous ambulatory peritoneal dialysis (CAPD) using bottles was 5.5 episodes per year at risk. Treatment was intraperitoneal cefazolin at 125 mg/L dialysis fluid. An aminoglycoside (gentamicin or tobramycin) was added at a dose of 4–8 mg/L if Gram-negative infection was suspected. The catheter was removed in the presence of fungal peritonitis, peritonitis with a tunnel infection, and cloudy effluent after 3 days of appropriate antibiotic treatment. Within 2 years with increased experience and use of bags instead of bottles for the dialysis fluid, the peritonitis rate had decreased to one episode per year at risk. With the subsequent development of new technologies, including the Y set, the flush before fill technique, improved training, improved care of the exit site of the PD catheter, and better adherence to that International Society of Peritoneal Dialysis (ISPD) guidelines, peritonitis rates have fallen in many programs to 0.3 episodes per year at risk. In our program over the last 5 years, the peritonitis rate is 0.17 episodes per year at risk, with a rate of 0.04 episodes of coagulase-negative Staphylococcus per year at risk. Therefore, there has been considerable success in lowering peritonitis occurrence. However, much about treating peritonitis remains unknown and is on the basis of expert opinion rather than research.
How long after antibiotics do you get peritonitis?
Cho and Johnson ( 5) have shown that the risk of repeat peritonitis, defined as peritonitis with the same organism >4 weeks after completion of antibiotics for a previous episode, is highest in the 3 months after an episode but that the risk continues to >24 months.
Is intermittent dosing as effective as continuous dosing?
Intermittent dosing is as effective as continuous dosing. There is almost no evidence of appropriate timing of the removal of the PD catheter for severe peritonitis. The authors conclude that studies of treatment of peritonitis in patients on PD are limited, are generally of low quality, and use different definitions.
How important is paracentesis?
The importance of paracentesis was demonstrated in a review of a database of 17,711 patients with cirrhosis and ascites who were admitted to the hospital with a primary diagnosis of ascites or encephalopathy [ 5 ]. Paracentesis was performed in 61 percent. Patients who underwent paracentesis had a lower in-hospital mortality rate than those who did not undergo paracentesis (6.5 versus 8.5 percent; adjusted odds ratio 0.55, 95% CI 0.41-0.74).
Should paracentesis be performed in patients with suspected SBP?
Paracentesis should be carried out promptly in patients with suspected SBP, as delays in performing paracentesis have been associated with increased mortality. (See 'Paracentesis' below and "Spontaneous bacterial peritonitis in adults: Clinical manifestations", section on 'Clinical manifestations' and "Diagnostic and therapeutic abdominal ...