Although the exact mechanism of action of macrolides is not clear, it has been hypothesized that macrolides show their action by blocking protein synthesis in bacteria in the following ways:
- Preventing the Transfer of the Peptidyl tRNA from the A-site to the P-site.
- Promotion of Peptidal tRNA Dissociation
- Blocking Peptidyl Transferase.
- Preventing Ribosomal Assembly
What is the mechanism of action of macrolide antibiotics?
Macrolide Resistance The antimicrobial activity of macrolides is based on inhibition of bacterial protein biosynthesis after binding of the macrolide, selectively and reversibly, to the 50S ribosomal subunit.
How do macrolides work?
Mechanisms of action and clinical application of macrolides as immunomodulatory medications Macrolides have diverse biological activities and an ability to modulate inflammation and immunity in eukaryotes without affecting homeostatic immunity.
How do macrolides block protein synthesis in bacteria?
Although the exact mechanism of action of macrolides is not clear, it has been hypothesized that macrolides show their action by blocking protein synthesis in bacteria in the following ways: Preventing the Transfer of the Peptidyl tRNA from the A-site to the P-site. Promotion of Peptidal tRNA Dissociation. Blocking Peptidyl Transferase.
What is the mechanism of resistance to macrolides?
Macrolide Resistance. The methylation of the adenine at position 2058 of domain V prevents macrolides from binding to the ribosome, resulting in high-level resistance. The second is an active drug efflux mechanism, which is determined by the presence of the membrane-bound efflux protein, encoded by the mef (A) gene.

What do macrolide antibiotics do?
What are macrolides and how do they work? Macrolides are a class of antibiotic that includes erythromycin, roxithromycin, azithromycin and clarithromycin. They are useful in treating respiratory, skin, soft tissue, sexually transmitted, H. pylori and atypical mycobacterial infections.
What are the mechanism of antibacterial action and the antibacterial spectrum of macrolides?
Macrolides act as antibiotics by binding to bacterial 50S ribosomal subunit and interfering with protein synthesis.
What is the mechanism of resistance of macrolides?
Two principal mechanisms of resistance to macrolides have been identified in Gram-positive bacteria. Erythromycin-resistant methylase is encoded by erm genes. Resultant structural changes to rRNA prevent macrolide binding and allow synthesis of bacterial proteins to continue.
What is the classification of macrolides?
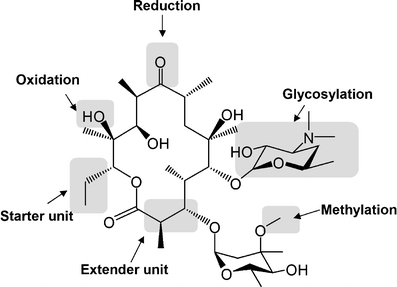
Macrolides, one of the most commonly used class of antibiotics, are a group of drugs produced by Streptomyces species. They belong to the polyketide class of natural products. Their activity is due to the presence of a large macrolide lactone ring with deoxy sugar moieties.
What are the 5 mechanisms of action of antimicrobial drugs?
Basis of Antimicrobial Action Various antimicrobial agents act by interfering with (1) cell wall synthesis, (2) plasma membrane integrity, (3) nucleic acid synthesis, (4) ribosomal function, and (5) folate synthesis.
What is the mechanism of action of azithromycin?
Mechanism of action Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA. Nucleic acid synthesis is not affected.
How are bacteria resistant to macrolides?
Bacteria resist macrolide and lincosamide antibiotics in 3 ways: (1) through target-site modification by methylation or mutation that prevents the binding of the antibiotic to its ribosomal target, (2) through efflux of the antibiotic, and (3) by drug inactivation.
Which of the following is a macrolide antibiotic?
Five macrolide antibiotics are currently available for use in the United States: erythromycin, clarithromycin, azithromycin, fidaxomicin and telithromycin, the latter being a related ketolide.
Is macrolides bacteriostatic or bactericidal?
[8] Macrolides are bacteriostatic agents as they only inhibit protein synthesis, although, at high doses, they can be bactericidal.
Why they are called macrolides?
What are Macrolides? Macrolides are a class of antibiotics derived from Saccharopolyspora erythraea (originally called Streptomyces erythreus), a type of soil-borne bacteria. Macrolides inhibit protein synthesis in bacteria by reversibly binding to the P site of the 50S unit of the ribosome.
When is a macrolide prescribed?
Macrolides are frequently prescribed for sinusitis, acute otitis media, and pharyngitis. However, macrolides are a suboptimal choice for treating these infections due to increasing levels of Streptococcus pneumoniae and group A Streptococcus macrolide resistance [6–8].
Is amoxicillin a macrolide?
Azithromycin is in the macrolide category of antibiotics, while amoxicillin is in the beta-lactam/penicillin category. They work in different ways and have some differences, such as in indications and drug interactions.
What are the six mechanisms of action of antibiotics?
There are six major modes of action: (1) interference with cell wall synthesis, (2) inhibition of protein synthesis, (3) interference with nucleic acid synthesis, (4) inhibition of a metabolic pathway, (5) inhibition of membrane function, (6) inhibition of ATP Synthase (Fig. 1).
Are macrolides broad spectrum?
The macrolides are bacteriostatic antibiotics with a broad spectrum of activity against many gram-positive bacteria.
What does the spectrum of activity of an antimicrobial indicate?
The antimicrobial spectrum of an antibiotic means the range of microorganisms it can kill or inhibit. Antibiotics can be divided into broad-spectrum antibiotics, extended-spectrum antibiotics and narrow-spectrum antibiotics based on their spectrum of activity.
Which of the following is the general mechanism of action for erythromycin?
Erythromycin acts by inhibition of protein synthesis by binding to the 23S ribosomal RNA molecule in the 50S subunit of ribosomes in susceptible bacterial organisms.
What are the side effects of macrolide?
Some of the most common side effects of macrolide are nausea, vomiting, and diarrhea. Severe side effects include anaphylaxis, permanent sensorineu...
What kind of drugs are macrolides?
Macrolides are antibiotics that are bacteriostatic in nature, which means, these antibiotics have the ability to inhibit the growth of bacteria. Ho...
What are examples of macrolide antibiotics?
Some of the common examples of macrolide antibiotics are erythromycin, clarithromycin, azithromycin, fidaxomicin, and telithromycin. Different dose...
What is a macrolide?
Macrolides are natural products which belong to the class of polyketides. Macrolides (such as erythromycin, azithromycin, clarithromycin, dirithromycin, troleandomycin, etc.) are useful in treatment of infections caused by gram-positive bacteria.
What is macrolide antibiotic?
The macrolides are considered to be slightly broad-spectrum antibiotics when compared to penicillins and are commonly used in place of penicillin in patients which demonstrate allergic symptoms to penicillin. Clinically macrolides are the most important class of antibiotics.
Where do macrolides bind?
The macrolide antibiotics seem to bind at the P-site of the 50S ribosomal subunit. As a result of which, during translation, the P-site is occupied by the macrolide. When the t-RNA attached with the peptide chain tries to move to the P-site, it cannot go there due to the presence of the macrolide, thus getting thrown away. This prevents the transfer of the peptidyl tRNA from the A-site to the P-site and blocks the protein synthesis due to the inhibition of the translocation of the nascent peptide chain. The macrolides also promote the premature dissociation of the peptidal tRNA from the A-site.
Which subunit of ribosomes do macrolides bind to?
The transcript of the animation is as follows: ” The macrolides bind reversibly to the 50S subunit of bacterial ribosomes. There is evidence that some prevent the transfer of the peptidyl tRNA from the A-site to the P-site, thus preventing the elongation of the polypeptide chain. “.
What prevents ribosome assembly?
Preventing Ribosomal Assembly. Research has shown that in the presence of macrolides, the amount of free 50S ribosomal subunits increases within bacterial cells, which lead to the hypothesis that macrolides prevented the assembly of the ribosomes in bacterial cells and also caused bacterial cell death.
Which enzyme is responsible for the formation of peptide bonds between the amino acids located on the A-site and the?
Macrolides bind to the P-site of the 50S ribosomal RNA and also block the action of the enzyme peptidyl transferase. This enzyme is responsible for the formation of the peptide bonds between the amino acids located on the A-site and the P-site in the ribosome.
How many atoms are in a macrocyclic lactone ring?
Mechanism of Action of Macrolides. Macrolides are antibiotics which consists of a large macrocyclic lactone ring (generally consisting of 12-17 atoms in the ring) to which are attached deoxy sugars.
How do macrolides work?
The mechanism of action of macrolides revolves around their ability to bind the bacterial 50S ribosomal subunit causing the cessation of bacterial protein synthesis. Once bound, the drug prevents the translation of mRNA, specifically the growing peptide chain, by preventing the addition of the next amino acid by the tRNA. Since the bacterial ribosomal structure is highly conserved across most, if not all, bacterial species, it is considered to be broad-spectrum.[7] Macrolides are considered to be bacteriostatic as they only inhibit protein synthesis, although, at high doses, they can be bactericidal.
What is a macrolide?
Macrolides - StatPearls - NCBI Bookshelf. Macrolides are a class of drugs used in the management and treatment of various bacterial infections. This activity reviews the mechanism of action, indications, contraindications, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, ...
Why are macrolides resistant to antibiotics?
Due to the overprescription of antibiotics, there has been tremendous growth in resistance to many mainstay therapies. Macrolides are no exception to this, and many organisms are excessively resistant to them. Studies show a strong link to genetic mutations in bacteria and the ability to spread these genes via transposable elements. The gene in question allows bacteria to be resistant to macrolides, lincosamides, and streptogramin groups of antibiotics at once. [8]
Why are macrolides used in COPD?
The use of these drugs in COPD is because of their anti-inflammatory and immunomodulating characteristics. [6] Mechanism of Action.
What is macrolide therapy?
Macrolides are a class of drugs used in the management and treatment of various bacterial infections. This activity reviews the mechanism of action, indications, contraindications, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant interactions) related to macrolides. NCBI.
Which antibiotic has the highest tendency to cause ventricular fibrillation?
Erythromycin has the highest tendency, and azithromycin has the lowest. The increase in the intervals puts patients at risk of cardiac arrhythmias like Torsades de pointes, ventricular tachycardia, and ventricular fibrillation. The most common arrhythmia arising from the use of macrolides would be Torsades de Pointes.
Can macrolides cause nausea?
Like any other antibiotic, macrolides carry a significant risk of typical adverse effects like nausea, vomiting , abdominal pain, and diarrhea. Abdominal symptoms are largely the result of macrolides being motilin agonists causing an increased risk of gastrointestinal upset and side effects.[9] .
What is a macrolide?
The 14-, 15-, and 16-membered macrolides are a widely used family of antibiotics. They have excellent tissue penetration and antimicrobial activity, mainly against Gram-positive cocci and atypical pathogens (27). Macrolide concentrations are at least 10-fold higher in the epithelial lung fluid than in serum. Erythromycin A, a 14-membered macrolide, was isolated more than 50 years ago from cultures of Streptomycesand was the first macrolide introduced into clinical practice (183, 325). In this review, macrolide antibiotics are called “macrolides.”
How do macrolides help with inflammation?
Summary: Macrolides have diverse biological activities and an ability to modulate inflammation and immunity in eukaryotes without affecting homeostatic immunity. These properties have led to their long-term use in treating neutrophil-dominated inflammation in diffuse panbronchiolitis, bronchiectasis, rhinosinusitis, and cystic fibrosis. These immunomodulatory activities appear to be polymodal, but evidence suggests that many of these effects are due to inhibition of extracellular signal-regulated kinase 1/2 (ERK1/2) phosphorylation and nuclear factor kappa B (NF-κB) activation. Macrolides accumulate within cells, suggesting that they may associate with receptors or carriers responsible for the regulation of cell cycle and immunity. A concern is that long-term use of macrolides increases the emergence of antimicrobial resistance. Nonantimicrobial macrolides are now in development as potential immunomodulatory therapies.
How long does erythromycin help with DPB?
aeruginosa(213). In subjects with DPB, treatment with erythromycin or roxithromycin for up to 24 months decreased IL-1β, IL-8, and neutrophils in BAL fluid (244). Other studies have shown that macrolides suppress proinflammatory cytokines in human airway washings and in serum (17, 133, 135, 198, 283).
How effective are macrolides?
The nonantimicrobial properties of macrolides were suspected as far back as the 1960s (110), but their dramatic clinical effectiveness in treating diffuse panbronchiolitis (DPB) has served to extend their use to a number of chronic inflammatory diseases (71, 157, 202). DPB is a chronic debilitating disorder of unknown etiology primarily afflicting East Asians and resulting in refractory airway infection and life-threatening chronic respiratory failure. By helping to resolve unregulated and destructive inflammation, macrolides increased the 10-year survival rate from <40% in 1970 to 1979 to >90% after the widespread use of chronic erythromycin therapy (157). The characteristics of the clinical response to macrolide therapy are summarized as follows (71, 157, 202, 258): (i) it takes up to 3 months of therapy for macrolides to show a significant effect; (ii) doses that are much lower than the MIC (i.e., low-dose macrolide therapy) are effective; (iii) the effect is seen even when patients are infected with macrolide-resistant bacteria, such as Pseudomonas; (iv) clinical improvement is recognized even when bacteria persist in posttreatment sputum; and (v) these actions are seen only for treatment with 14- and 15-membered macrolides (e.g., erythromycin, clarithromycin, roxithromycin, and azithromycin), not with the 16-membered macrolide antibiotics (120). The effects of macrolides in patients with chronic inflammatory airway disease appear to be independent of antimicrobial properties. Immunomodulation, which differs from immunosuppression or anti-inflammation, is a nonlinear resetting of the inflammatory response by modifying or regulating one or more functions of the immune system (238). We use the term “immunomodulation” to describe the downregulation of a hyperimmunity or hyperinflammation without impairing the normal immune or inflammatory response to defend against infection.
What is the main cell that produces mucin?
Airway mucin is synthesized by epithelial goblet cells and by mucous cells of the submucosal glands. MUC5AC and MUC5B are the major gel-forming mucins in the human airway (281, 316, 317). Shimizu et al. (254) documented that erythromycin and clarithromycin inhibit tumor necrosis factor alpha (TNF-α)-induced mucus secretion in a dose- and time-dependent manner in NCI-H292 cells (a human mucoepidermal cell line) and in nasal epithelial cells. This effect is accompanied by a reduced expression of MUC5AC mRNA. Immunohistochemistry showed that clarithromycin and roxithromycin inhibit mucus production induced by ovalbumin (OVA) instillation in OVA-sensitized rats or by lipopolysaccharide (LPS) exposure in rats (216, 254). Similar results were obtained after Pseudomonas aeruginosainfection in mice (125). In this investigation, clarithromycin inhibited mucus production and extracellular signal-regulated kinase 1/2 (ERK1/2) phosphorylation in the lungs of Pseudomonas aeruginosa-infected mice.
How do macrolides affect neutrophil chemotaxis?
It is likely that the effects of macrolides on neutrophil chemotaxis are due to decreased production of chemoattractants and decreased expression of adhesion molecules (97, 285).
What molecule stimulates MUC5AC?
The P. aeruginosaautoinducer N-3-oxododecanoyl homoserine lactone (3-oxo-C12-HSL), a quorum sensing signal molecule, also stimulates the production of MUC5AC in NCI-H292 cells, through ERK1/2 and IκB phosphorylation (105). This induction was suppressed by azithromycin, and 3-oxo-C12-HSL-induced MUC5AC production was blocked by the ERK pathway inhibitor PD98059. Similarly, stimulation of cells with LPS or transforming growth factor alpha (TGF-α) induces phosphorylation of IκBα (285). Macrolides inhibited LPS-induced MUC5AC gene expression and attenuated TGF-α-induced and LPS-induced phosphorylation of IκBα.
How do macrolides exert their antibiotic effect?
Macrolides exert their antibiotic effect by binding irreversibly to the 50S subunit of bacterial ribosomes. Ribosomes are the protein factories of the cell, and by binding to the ribosome, macrolides inhibit translocation of t RNA during
What type of infection are macrolides used for?
Type of Infections Macrolides Are Used Against. Macrolide antibiotics are used to treat infections of the respiratory tract, genital, gastrointestinal tract, and soft tissue infections caused by strains of bacteria susceptible to this class of antibiotics.
What is virtual microbiology classroom?
The Virtual Microbiology Classroom provides a wide range of free educational resources including PowerPoint Lectures, Study Guides, Review Questions and Practice Test Questions.
Is a macrolide effective against a bacterium?
Like penicillin, these drugs are effective against beta-hemolytic Streptococci, pneumococci, Staphylococci and Enterococci. Macrolides are, however, effective against a slightly wider range of bacteria than is penicillin, including Mycoplasma , Mycobacteria, some rickettsia and chlamydia.
Is a macrolide bactericidal or bacteriostatic?
This action is mainly bacteriostatic, meaning that bacterial growth and reproduction are inhibited, in contrast to bactericidal antibiotics which directly kill bacteria. Macrolides can be bactericidal in high concentrations.
How do macrolides work?from ncbi.nlm.nih.gov
The mechanism of action of macrolides revolves around their ability to bind the bacterial 50S ribosomal subunit causing the cessation of bacterial protein synthesis. Once bound, the drug prevents the translation of mRNA, specifically the growing peptide chain, by preventing the addition of the next amino acid by the tRNA. Since the bacterial ribosomal structure is highly conserved across most, if not all, bacterial species, it is considered to be broad-spectrum.[7] Macrolides are considered to be bacteriostatic as they only inhibit protein synthesis, although, at high doses, they can be bactericidal.
How do macrolides affect immune system?from pubmed.ncbi.nlm.nih.gov
Macrolides have diverse biological activities and an ability to modulate inflammation and immunity in eukaryotes without affecting homeostatic immunity. These properties have led to their long-term use in treating neutrophil-dominated inflammation in diffuse panbronchiolitis, bronchiectasis, rhinosinusitis, and cystic fibrosis. These immunomodulatory activities appear to be polymodal, but evidence suggests that many of these effects are due to inhibition of extracellular signal-regulated kinase 1/2 (ERK1/2) phosphorylation and nuclear factor kappa B (NF-kappaB) activation. Macrolides accumulate within cells, suggesting that they may associate with receptors or carriers responsible for the regulation of cell cycle and immunity. A concern is that long-term use of macrolides increases the emergence of antimicrobial resistance. Nonantimicrobial macrolides are now in development as potential immunomodulatory therapies.
Why are macrolides resistant to antibiotics?from ncbi.nlm.nih.gov
Due to the overprescription of antibiotics, there has been tremendous growth in resistance to many mainstay therapies. Macrolides are no exception to this, and many organisms are excessively resistant to them. Studies show a strong link to genetic mutations in bacteria and the ability to spread these genes via transposable elements. The gene in question allows bacteria to be resistant to macrolides, lincosamides, and streptogramin groups of antibiotics at once. [8]
What are the effects of macrolides on macrophages?from ncbi.nlm.nih.gov
Later changes seen in macrophages that interact with macrolides include inhibition of cell function and cellular transport along with surface receptor expression regulation. All of these culminate in the immunomodulatory effects of macrolides in the body. [1]
Why are macrolides used in COPD?from ncbi.nlm.nih.gov
The use of these drugs in COPD is because of their anti-inflammatory and immunomodulating characteristics. [6] Mechanism of Action.
What is macrolide therapy?from ncbi.nlm.nih.gov
Macrolides are a class of drugs used in the management and treatment of various bacterial infections. This activity reviews the mechanism of action, indications, contraindications, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant interactions) related to macrolides. NCBI.
Which antibiotic has the highest tendency to cause ventricular fibrillation?from ncbi.nlm.nih.gov
Erythromycin has the highest tendency, and azithromycin has the lowest. The increase in the intervals puts patients at risk of cardiac arrhythmias like Torsades de pointes, ventricular tachycardia, and ventricular fibrillation. The most common arrhythmia arising from the use of macrolides would be Torsades de Pointes.
What is macrolide used for?
Macrolides are used in the treatment of a wide range of infections – both Gram-positive and Gram-negative infections. In the case of H. pylori infection, macrolides are used alongside other drugs – typically a penicillin and a proton-pump inhibitor (what is referred to as “ triple therapy ”).
What is macrolide antibiotic?
Antibacterial macrolides are widely prescribed drugs for an even wider variety of infections. Here, we review the macrolides pharmacology you need to know. We discuss the indications that macrolides are licensed to treat, how they work, what side effects they’re linked to, and what drug interactions you need to bear in mind.
How does fidaxomicin work?
Fidaxomicin is different, in that its actions are bactericidal, and it works by binding to the switch regions of RNA polymerase. Earlier macrolides had broader spectrum of activity. Erythromycin, for example, has relatively broad activity against both Gram-positive and Gram-negative organisms.
Why do bacteria resist macrolides?
However, bacterial resistance to macrolides is relatively common, often caused by mutations within the ribosome that prevent the macrolide from binding.
Which subunit does macrolides bind to?
More specifically, macrolides bind to the 50S ribosomal subunit; binding that results in blockade of the translocation process which is needed for the polypeptide chain to grow and elongate.
Can macrolides prolong QT?
QT prolongation. At high doses, macrolides can cause ototoxicity. QT prolongation is more likely if macrolides are administered along side other drugs that also prolong the QT interval – such as SSRIs, antipsychotics, quinine, and fluoroquinolones.
Can you use macrolides for Helicobacter pylori?
Eradication of Helicobacter pylori infection. In the case of H. pylori infection, macrolides are used alongside other drugs – typically a penicillin and a proton-pump inhibitor (what is referred to as “ triple therapy ”). Patients who are allergic to penicillins can be given metronidazole instead.
